An Updated Overview of Low Back Pain Management
Article information
Abstract
We aimed to determine the recommendation level for the treatment of acute and chronic low back pain (LBP). A systematic review (SR) of the literature was performed and all English-language articles that discuss acute and chronic LBP, including MEDLINE and the Cochrane Database of Systematic Reviews, were searched. Of the 873 searched literature reports, 259 articles, including 131 clinical trials, 115 SRs, nine meta-analyses, and four clinical guidelines were analyzed. In these articles, high-quality randomized controlled trials, SRs, and used well-written clinical guidelines were reviewed. The results indicated multiple acute and chronic LBP treatment methods in the literature, and these reports when reviewed included general behavior, pharmacological therapy, psychological therapy, specific exercise, active rehabilitation and educational interventions, manual therapy, physical modalities, and invasive procedures. The Trial conclusions and SRs were classified into four categories of A, B, C, and D. If there were not enough high-quality articles, it was designated as “I” (insufficient). This review and summary of guidelines may be beneficial for physicians to better understand and make recommendations in primary care.
Introduction
The lifetime prevalence of low back pain (LBP) is over 70% in industrialized countries with a worldwide lifetime prevalence of 84% [1,2]. Accordingly, many guidelines for treating LBP have been published in the past 20 years. Most of the current guidelines focus on the use of medications [3–6]. Acute and chronic LBP are completely different manifestations of pain that must be treated differently. Acute LBP is prevalent and may transition into chronic LBP, which is associated with reduced quality of life, pain, and disability [7]. Acute LBP can be treated conservatively at first and certain physical therapy approaches usually exacerbate rather than help the condition. To identify patients who are likely going to require more complex triage and prolonged therapies should be performed compared to those whose back pain would resolve spontaneously. Therefore, selective adoption of certain treatment modalities is required for physicians in the treatment of acute and chronic LBP.
We previously published preliminary guidelines for LBP that focused on medication in 2017 [8]. There were many limitations in it; thus, we thoroughly reviewed the comprehensive treatment modalities and approaches, then graded the approach accordingly, which focused on general behavior, pharmacological and psychological therapy, exercise, rehabilitation, educational intervention, physical modalities, and invasive procedures [9]. We reviewed the previous guidelines and perused high-quality articles to determine the recommendations for acute as well as chronic conditions with multiple treatment modalities. This review may enhance the recommendations in the current guidelines regarding LBP treatment.
Methods
1. Data sources and searches
We searched articles on acute and chronic LBP, including the MEDLINE database and the Cochrane Database of Systematic Reviews for relevant reviews. A comprehensive literature search was conducted from 1980 to 2019. The inclusion criteria were studies with LBP but studies on LBP associated with neuropathic pain were excluded. We also excluded reviews that were outdated and did not use clear systematic methods and systematic reviews (SRs) that evaluated target medications but did not report targeted results for patients with LBP. Our primary source for trials was the review of clinical guidelines, SRs, and meta-analyses because of the large number of trials that have evaluated medications for LBP. Additionally, searches for high-quality randomized controlled trials (RCTs), particularly when there was insufficient data for treatment modalities, were conducted. Institutional review board approval was not necessary for this study at Korea University Ansan Hospital.
2. Data extraction
An expert panel determined the treatments to be included in this review. Data were subsequently abstracted by reviewers and thereby verified. For each trial, acute LBP (less than 4 weeks in duration) and chronic/subacute LBP (greater than 4 weeks in duration) were differentiated. If specific data on the duration of trials were not provided, the categorization (acute or chronic/subacute) assigned by the articles was relied upon.
3. Quality assessment
Internal validity, including the quality of SRs, was assessed by the Scottish Intercollegiate Guidelines Network criteria [10]. The Methodology Checklist can be applied to six different types comprising of SRs, RCTs, observational studies, diagnostic studies, economic studies, and patient issues. After the assessment of validity, the overall assessment was evaluated using three options. Two independent raters (J.Y.H. and J.H.C.) then conducted the quality assessment.
4. Analysis of evidence and recommendations
The analysis of evidence and recommendations followed the Systems to Rate the Strength of Scientific Evidence of the Agency for Healthcare Research and Quality [10]. The evidence in each article was categorized from 1++ (which is most highly qualified) to 4 (which is most poorly qualified). Recommendation grades for treatment modalities were determined in the expert panel discussion consistent with the strength of the evidence. Conclusions of the trials and SRs were classified as A, B, C, and D. If there were not enough numbers of high-quality articles, it was classified as insufficient (I) (Table 1). The final verdict regarding the recommendation grade using each approach was obtained according to the agreement of the four raters (J.Y.H., J.H.L., K.S.S., and J.H.L.)
Results
Out of the 873 searched literature reports, 869 abstracts of those articles were reviewed; 427 articles were excluded after reviewing the abstract. The remaining 442 articles were reviewed by the study panel group during which 187 articles were excluded after quality evaluation. In summary, 259 articles including 131 clinical trials, 115 SRs, nine meta-analyses, and four clinical guideline reviews were analyzed. In these articles, the high-quality RCTs, SRs, and well-written clinical guideline reviews were reviewed (Fig. 1).
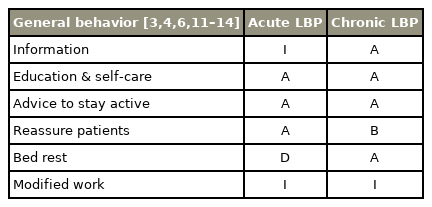
1. General behavior
A variety of acute and chronic LBP treatment methods are seen in the literature and these methods were reviewed accordingly (Table 2). Four trials found that effective treatment included education in addition to self-care and also recommendations for multiple activities for patients that had acute LBP. Furthermore, we found three positive clinical guidelines, which strongly support the LBP improvement while reassuring patients and guiding acute LBP [4,6,11–14]. However, sufficient evidence for bed rest and modified work recommendations were not found. For chronic LBP, two higher-quality trials, which showed evidence for education, self-care, and recommendations for staying active were acquired [3,4,12,13]. Moreover, two clinical guidelines that strongly support reassuring patients and bed rest for treating chronic LBP were attained.
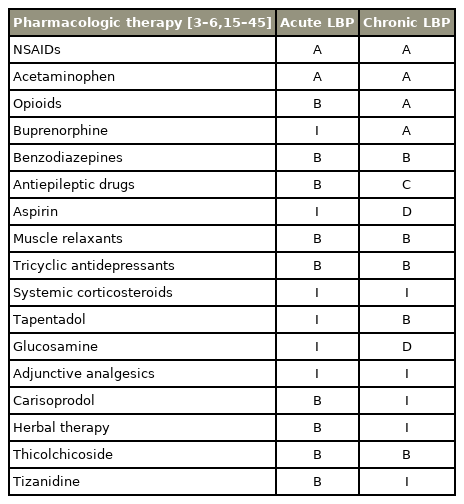
2. Pharmacologic therapy
Multiple higher-quality trials, SRs, and numerous clinical guidelines have demonstrated improvement with nonsteroidal anti-inflammatory drugs (NSAIDs) acetaminophen (AAP), and paracetamol for acute LBP [15–24] (Table 3). Two trials and one clinical guideline reported minimal evidence for carisoprodol, herbal therapy, thiocolchicoside, and tizanidine [6,16,18]. Additionally, LBP improvement with opioids, benzodiazepines, muscle relaxants, and tricyclic antidepressants in two high-quality systemic reviews and three clinical guidelines has been reported [4–6,24]. There were several higher-quality trials and SRs that support the pain improvement of NSAIDs, AAP, paracetamol, opioids, and buprenorphine in chronic LBP [3,4,6,17,21–45]. Benzodiazepines, muscle relaxants, tricyclic antidepressants, tapentadol, and pregabalin were supported by seven higher-quality studies and also three clinical guidelines reported improvement in symptoms [3,4,6,39–45].
3. Psychological therapy
Two methods for treating acute and chronic LBP were included in this study (cognitive-behavioral therapy along with multidisciplinary treatment). No high-quality trials were found and general evidence from literature was insufficient to support the evidence of psychological therapy for acute LBP (Table 4). However, for chronic LBP, five high-quality trials reported pain improvement with cognitive-behavioral therapy [32,46–49]. Progressive muscle relaxation and multidisciplinary treatment were strongly supported by clinical guidelines, and the study methods were of a higher quality. Three clinical guidelines that strongly support the pain improvement of cognitive-behavioral therapy for chronic LBP were noticed [3,5,6].
4. Exercise
We identified general exercise and ten specific exercises for acute and chronic LBP in the literature. For acute LBP, six trials of general behavior and two clinical guidelines were reviewed to determine the effects of general exercise [4,6,50–54] (Table 4). The strategic method (action, sequence, use of tools, etc.), was defined as a specific exercise. After considering several trials and clinical guidelines, the results were insufficient to support pain improvement with the majority of specific exercises. Twelve higher-quality trials showed a significant difference in pain relief with general exercise for chronic LBP [47,48,50,55–59]. Consequently, it was determined the recommendation grade of general exercise based on two meta-analyses, three SRs, and three clinical guidelines for chronic LBP [3,4,6,60–64]. Seven trials, which supported stabilizing exercise for pain relief (which included two trials) and two clinical guidelines for aquatic and supervised exercise therapy were noted [3,5,34,46,65–71]. Moreover, one higher-quality trial, one meta-analysis, and two clinical guidelines found that yoga was an effective treatment [3,6,72,73]. However, several of these treatments were not supported by trials or analysis.
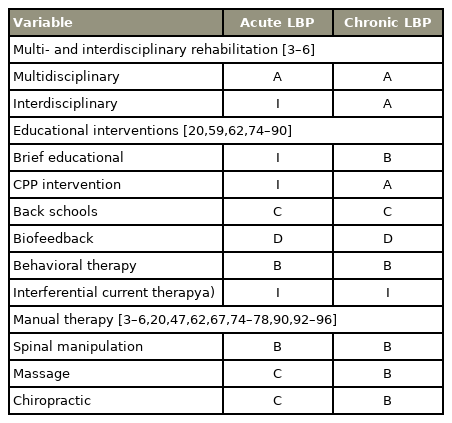
5. Multidisciplinary rehabilitation and educational interventions
Mutidisciplinary and interdisciplinary rehabilitation, as well as educational treatment methods for acute and chronic LBP were reviewed [3–6,20,59,62,74–90]. For acute LBP, an insufficient number of trials for the eight treatment methods were noted; however, two clinical guidelines were included [4,6] (Table 5). Twelve trials reported clear differences in pain relief with active rehabilitation followed by educational interventions for chronic LBP [59,79–88]. Six randomized trials, one SR, and three clinical guidelines for multidisciplinary rehabilitation for chronic LBP were identified [3–5,62,79–84]. Besides, six higher-quality trials and three clinical guidelines supported pain improvement with back schools [3,4,6,59,79–88].
6. Manual therapy
We reviewed spinal manipulation, mobilization, massage, and chiropractic management for treating acute as well as chronic LBP. There was sufficient evidence from several RCTs along with clinical guidelines to support the improvement of pain in manual therapy in acute or chronic LBP [3–6,20,47,62,67,74–77,90–96] (Table 5). For acute LBP, spinal manipulations were supported by three high-quality trials, one SR, in addition to two clinical guidelines [3,6,20,74,75,96]. For chronic LBP, four higher-quality trials, two SRs, as well as four clinical guidelines found evidence to support pain improvement with spinal manipulation [3–5,47,62,67,90,91,96]. Besides, three moderate quality trials supported pain improvement with chiropractic approaches for treating chronic LBP [76,94,95].
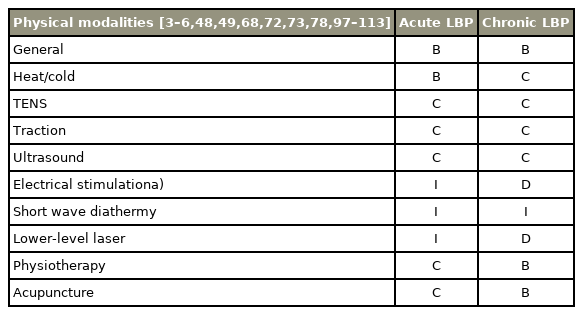
7. Physical modalities
Methods for treating acute and chronic LBP were reviewed [3–6,48,49,68,72,73,78,97–111] (Table 6). For acute LBP, the evidence from several trials plus clinical guidelines was insufficient to support pain improvement with the majority of physical modalities. One systemic review together with two clinical guidelines were included in the review of heat and cold therapy for acute LBP [4,6,49]. For chronic LBP, one higher-quality randomized trial supported pain improvement from general physical modalities [3,6,72,73,98]. Higher-quality trials, a SR, and three clinical guidelines that supported acupuncture for treating chronic LBP were observed [3,4,6,112,113]. Nevertheless, there was insufficient evidence for a majority of treatment methods for chronic LBP.
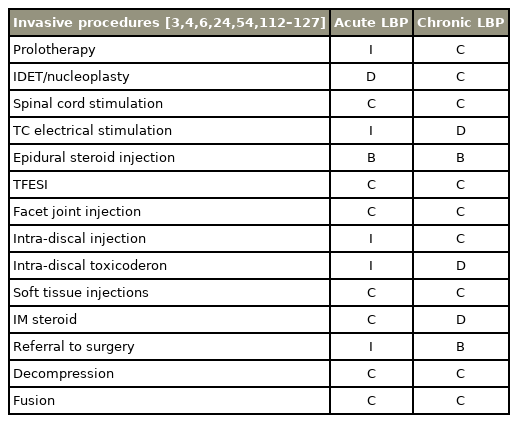
8. Invasive procedures
Methods for treating acute and chronic LBP were reviewed with invasive procedures (Table 7). There was insufficient evidence for the greater part of treatment methods for acute LBP [3,4,6,24,54,112–127]. There was a SR and another clinical guideline that supported an epidural steroid injection for treating acute LBP [4,24]. For chronic LBP, numerous clinical trials reported a variety of invasive treatments [3,4,6,112,113,127]. Furthermore, three higher-quality trials, one meta-analysis, one SR, and two clinical guidelines supported pain improvement with epidural steroid injection [3,4,24,116–118,126]. Nonetheless, there was insufficient evidence for surgery as a treatment for chronic LBP.
Discussion
Presently, there are various guidelines for treating LBP that have been published by professional committees, which have provided unpredictable types of recommendations. These study groups have adopted different weighting systems and several types of evidence to support present recommendations [3–6,128–132]. Common recommendations include diagnostic steps for patients with LBP, minimal use of radiographs, support of progressive activation, and opposition to bed rest. Nevertheless, many clinical guidelines have focused on pharmaceutical treatments, physical therapy settings, or specific subgroups of patients with radicular pain. Selected clinical guidelines have focused on secondary care, which includes occupational care of patients with radicular pain that is related to compression of the spinal nerves. Conversely, careful diagnostic differentiation is required; in primary care, diagnostic triage of LBP is the anchor for a diagnosis. Focused history and clinical examination are the initial steps, followed by subsequent workup and referral to medical specialist is the next step. The main goal of diagnostic triage of LBP is to exclude nonspinal causes in addition to allocating patients to one of three broad categories: specific spinal pathology (<1%), radicular syndrome (5%–10%) or nonspecific LBP, which represents 90%–95% of cases and is diagnosed by exclusion of the first two categories [133]. For specific spinal pathologies (e.g., vertebral fracture, malignancy, infection, axial spondyloarthritis, or cauda equina syndrome), a clinical assessment with computed tomography (CT) or magnetic resonance imaging (MRI) may reveal the key alerting features [134,135].
In this study, key treatment modalities and approaches that focused on general behavior, pharmacological therapy, psychological therapy, exercise, rehabilitation, educational intervention, physical modalities, and invasive procedures were reviewed. Although multiple clinical guidelines have reported insufficient evidence for surgical treatment, it does not eliminate the possibility that individual patients may benefit from surgical interventions. Additional guidance with appropriate surgical or interventional management is still needed, especially for chronic LBP and invasive procedures. Moreover, the duration of pain should be gravely considered in determining the recommendation level. As there are currently many different clinical guidelines, it was challenging to differentiate the treatment modalities for acute as well as chronic LBP. The published guidelines in addition to high-quality research articles to confirm recommendations for acute and chronic LBP were reviewed. Multiple treatment modalities, including invasive procedures for both acute and chronic LBP were also reviewed.
1. General behavior & pharmacologic therapy
In terms of general behavior, many high-quality trials found that effective treatment included education, self-care, and recommendations for activity for patients that had acute and chronic LBP. However, sufficient evidence was not found for improvement of pain with modified work. Further review is needed to confirm this recommendation. Physicians commonly apply pharmacological therapy with LBP and many higher-quality trials, SRs, and clinical guidelines with LBP improvement for NSAIDs, AAP for acute as well as chronic LBP were found. Many guidelines recommend that paracetamol should be used first and that nonsteroidal anti-inflammatory preparations can be used as a second course of treatment. Correspondingly, it was found that paracetamol and NSAIDs were associated with significant pain relief for acute and chronic LBP [15–24]. Moderate to high-quality trials that support the usage of benzodiazepines, muscle relaxants, tricyclic antidepressants, and thiocolchicoside with acute and chronic LBP were also noted. This group was given a grade B. An insufficient number of trials show improvement of pain with several medicines, and thus could not determine a recommendation grade for it. There is presently more evidence for second line drugs, including antidepressants, opioids, and benzodiazepines. However, these results are inconsistent with previous guidelines and reviews, showing a range of effectiveness with acute and chronic LBP. In terms of the duration of the pain, recommended drugs for acute LBP do not show similar effects for chronic LBP. Opioids and buprenorphine do not show similar pain improvements in the treatment of chronic LBP, which is beneficial to prevent opioid addiction in the LBP population. Otherwise, several drugs only showed pain relief in acute or chronic pain as a follow-up. There were multiple drugs with insufficient evidence to determine recommendation grades, which was a limitation of this study; further review is needed to confirm it.
2. Psychological therapy & exercise
Cognitive-behavioral therapy and multidisciplinary treatment for chronic LBP are recommended. General and aerobic exercises were recommended for chronic LBP with less evidence of pain improvement in acute LBP. Guideline development committees have included content from other guidelines. For example, several trials found distinct differences in pain relief with general exercise for general LBP [47,48,50,55–59]. Nevertheless, due to the lack of specification, it could not be determined whether these treatment options were effective for chronic LBP. In terms of specific exercise recommendations, specific back exercises are not recommended with acute LBP in the majority of guidelines. Conversely, back exercises have been recommended in chronic LBP. In this study, we showed that general and supervised exercises are recommended for chronic LBP treatment but not for acute LBP treatment. However, a patient’s severity of symptoms may determine whether or not it is available for acute pain. We moderately recommend supervised exercise, balanced exercise, and yoga for chronic LBP. In contrast, we could not determine a recommendation grade in a majority of specific exercises for acute LBP. There were multiple treatment modalities with insufficient evidence grades, which was a limitation. Although we found numerous specific exercises in trials and guidelines, high-quality articles strongly support that it was not available. Thus, further study is required to determine recommendations
3. Disciplinary rehabilitation, educational interventions, and manual therapy
We strongly recommended multidisciplinary and interdisciplinary rehabilitation for acute as well as chronic LBP. Even though there were insufficient trials this does not imply it should not be used. Consequently, physicians may expect pain improvement with disciplinary rehabilitation treatment in a clinical setting. Brief educational intervention, Child-Parent Psychotherapy intervention, and behavioral therapy were commended for chronic LBP with sufficient evidence but its use in acute LBP could not be determined. This is a limitation of our study, and further review is necessary for educational interventions in acute LBP treatment. Inappropriate beliefs and behaviors about acute LBP may induce as well as increase chronic pain; therefore, clinicians should recommend a combination of education and behavioral therapies [11–14]. Physicians can apply manual therapy in patients with acute and chronic LBP since it may be beneficial for certain groups of patients. Nevertheless, the evidence level was moderate to low and we gave this group grades B to C in this study.
4. Physical modalities and invasive procedures
General physical modalities were proposed in acute and chronic LBP. Nonetheless, there were a variety of specific physical modalities with insufficient evidence for use or were marginally recommended (grade B to C). We found several moderate to high-quality trials for the use of physiotherapy and acupuncture in chronic LBP. It was assigned as grade B. Conversely, sufficient evidence for improvement of pain with electrical stimulation, short wave diathermy, and lower-level laser treatment in acute LBP treatment were not noticed. Recently, various studies have been published with invasive procedures showing fair evidence, which may change the status with treatment of acute and chronic LBP [3,4,6,112,113,127,136]. Nonetheless, invasive procedures were not strongly suggested for LBP (grade C to D) and several trials for use of epidural steroid injection (grade B) were found in this study. Physicians can selectively refer patients to the surgical department (grade B) if chronic pain persists for a long time without any improvements. However, this does not mean surgical treatment is highly recommended for chronic LBP. These recommendations should be centered on assessments that exclude potentially serious spinal pathology or specific causes of LBP that may need surgical treatment. As a result, simple back pain and pathologic neuropathy with substantial neurologic involvement that could require an MRI or CT to confirm the diagnosis were separated. Invasive treatment may be needed to resolve the symptoms with spinal pathology.
5. Limitation of the study
We only focused on therapeutics, prevention (education), and rehabilitation in treatment of LBP. However, without a proper diagnosis of the LBP appropriate management cannot be instituted. Diagnostic triage is an essential recommendation for LBP, which is the most frequent musculoskeletal condition that general physicians encounter. In this study, differential diagnosis for red flag signs and indications for appropriate imaging procedures should have been included. Diagnostic triage in the updated overview for the management of LBP also could not be incorporated, which is a main limitation of the study.
Conclusions
High-quality trials and SRs were evaluated to assess the current recommendations for treating acute and chronic LBP. This review as well as the summary of guidelines may be beneficial for physicians to better understand and make recommendations for different degrees of LBP, particularly in primary care.
Notes
Conflict of Interest
No potential conflict of interest relevant to this article was reported.