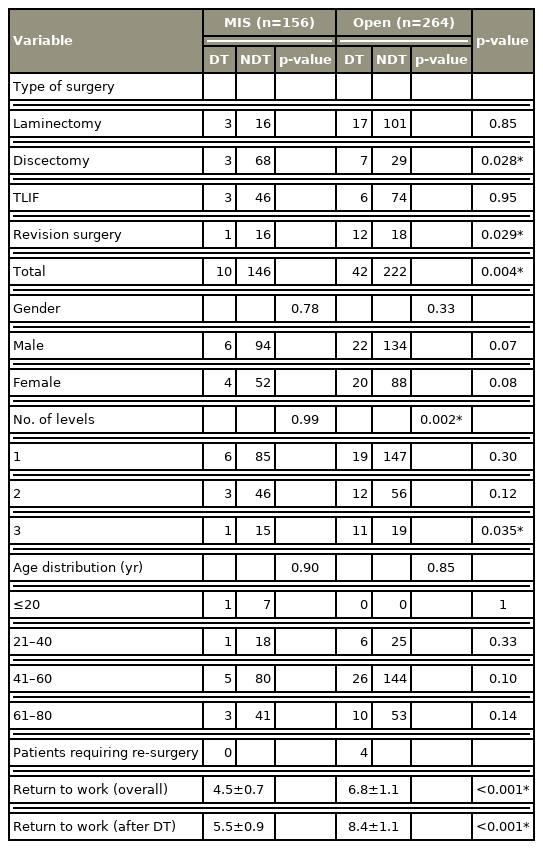
Incidence of Dural Tears in Open versus Minimally Invasive Spine Surgery: A Single-Center Prospective Study
Article information
Abstract
Study Design
A prospective comparative study.
Purpose
To compare the incidence of unintended durotomy and return to work after open surgery versus minimally invasive spine surgery (MIS) for degenerative lumbar pathologies.
Overview of Literature
The incidence of accidental durotomy varies between 0.3% and 35%. Most of these are from open surgeries, and only a handful of studies have involved the MIS approach. No single-center studies have compared open surgery with MIS, especially in the context of early return to work and dural tear (DT).
Methods
This study included 420 operated cases of degenerative lumbar pathology with a prospective follow-up of at least 6 months. Patients were divided into the open surgery and MIS groups, and the incidences of DT, early return to work, and various demographic and operative factors were compared.
Results
A total of 156 and 264 patients underwent MIS and open surgery, respectively. Incidental durotomy was documented in 52 cases (12.4%); this was significantly less in the MIS group versus the open surgery group (6.4% vs. 15.9%, p<0.05). In the open surgery group, four patients underwent revision for persistent dural leak or pseudomeningocele, but none of the cases in the MIS group had revision surgery due to DT-related complications. The incidence of DT was higher among patients with high body mass index, patients with diabetes mellitus, and patients who underwent revision surgery (p<0.05) regardless of the approach. The MIS group returned to work significantly earlier.
Conclusions
MIS was associated with a significantly lower incidence of DT and earlier return to work compared with open surgery among patients with degenerative lumbar pathology.
Introduction
Unintended durotomy remains the most common complication in degenerative lumbar spinal surgery, but its incidence in the literature widely varies, ranging from 0.3% to 35%, depending on the type of surgery [1–6]. Unintended durotomy can result in complications, such as postural headache, persistent dural leak, and pseudomeningocele formation [7–10]. In the last few decades, minimally invasive spine surgery (MIS) has become a popular approach for spine surgery. It has the advantage of a smaller incision and faster rehabilitation. However, it comes at the cost of limited visualization and a steeper learning curve. Considering all of these, the benefit of MIS in preventing complications, such as accidental durotomy, is still being debated. The proponents of MIS cite its advantages (i.e., muscle-sparing procedure, smaller incision, and less dead space) in preventing pseudomeningocele and persistent cerebrospinal fluid (CSF) leak following an incidental durotomy [10]. Despite the abundance of literature on unintended durotomy in both open surgery and MIS, the lack of matched cohorts makes it difficult to compare the results of the two approaches, and the limited number of cohort studies that are available are mostly retrospective in nature [11]. We could not find a single-center study with matched cohorts that compared both approaches. Herein, we present the first single-center prospective study to compare the incidence of unintended durotomy in open surgery versus MIS for degenerative lumbar pathology over a 34-month duration.
Materials and Methods
Between November 2017 and September 2020, a prospective cohort study was conducted among patients who underwent surgery for degenerative lumbar pathology at Bharatratna Dr Babasaheb Ambedkar Central Railway Hospital, Mumbai in Western India. The study was commenced after obtaining approval from the institutional ethics committee of Bharatratna Dr Babasaheb Ambedkar Central Railway Hospital, Mumbai (EC/BYC/11.10.2017/Dr.P.D). All patients who underwent degenerative lumbar spine surgery and who consented to be part of the study were included, and we obtained their written informed consent for sharing their clinical and radiological data. Patients who underwent surgeries for degenerative scoliosis and deformity correction, patients with pathologies at more than three levels, and patients who completed less than 6 months of follow-up duration were excluded from the study.
A total of 420 patients fulfilled the inclusion criteria. All patients were operated on by the same surgeon. For the first 12 months of the study period, patients exclusively underwent open surgery. In the next 6 months, both open surgery and MIS were employed, but only open surgeries were included in the study to remove potential bias from the learning curve of MIS. For the remaining 16 months, the MIS approach was exclusively used for all degenerative lumbar spinal pathologies, as the learning curve had been overcome. The data was classified into the open surgery and MIS groups, depending on the surgical approach. Data was also analyzed according to the type of surgical intervention. All cases were operated on under microscopic magnification by a single team of surgeons. Any disruption of dural integrity was considered a dural tear (DT). For DTs in open cases, primary repair was attempted using 5/0–6/0 Prolene. In irreparable DT, EVICEL Fibrin Sealant (Ethicon Inc., Somerville, NJ, USA) was used, and a fat pad was applied. For MIS cases, all DTs were managed using EVICEL Fibrin Sealant (Ethicon Inc.) and a layer of fat pad. The competency of the closure was confirmed in each case by asking the patient to perform the Valsalva maneuver before closure. We had a backup plan to convert the surgery to an open one in case the DT was large enough and required direct repair. Mobilization was delayed in all cases for 48 hours. Patients were kept in the Trendelenburg position and advised to lie prone according to their level of comfort. We did not use lumbar drain or acetazolamide in any case. All asymptomatic cases were mobilized after 48 hours. MIS discectomy and decompression were performed using an 18-mm tubular system, whereas a 22-mm tube was used for transforaminal lumbar interbody fusion (TLIF). All cases were periodically followed up for at least 6 months. Complications such as wound dehiscence, pseudomeningocele formation, were noted in the case record form. Return to work was noted in the follow-up visits, as well as any other complications reported by the patients.
Statistical analysis was conducted using IBM SPSS ver. 23.0 (IBM Corp., Armonk, NY, USA). Continuous variables were expressed as mean and variation of each observation from the mean value, represented as mean±standard deviation; these were analyzed using the independent t-test. Categorical variables were described by taking their percentages; these were analyzed using the chi-square test with Yates’ correction or Fisher’s exact test as appropriate. Intragroup variable analysis was conducted using the paired t-test, whereas multiple comparisons within groups were performed using the Sidak test. Statistical significance was set to p<0.05.
Results
The final analysis included 420 patients, with follow-up period ranging from 6 to 30 months. MIS was performed on 156 patients, whereas open surgery was performed on 264 patients. In our study, majority of the study participants were within the age group of 41–60 years (54.5% of MIS patients and 64.4% of open surgery patients), followed by 61–80 years, 21–40 years, and ≤20 years. The two groups were comparable in terms of age distribution, gender distribution, number of levels operated upon, duration of symptoms, distribution of BMI, comorbidities (i.e., hypertension and diabetes mellitus), and smoking (Table 1). Unintended durotomy was documented in 52 cases; 10 in the MIS group and 42 in the open surgery group. After failure of conservative treatment, four cases in the open surgery group had to undergo revision surgery due to persistent dural leak and pseudomeningocele formation (Figs. 1, 2). Two cases of delayed DT were noted in the open surgery group, wherein patients presented with symptoms of DT 1 month following open lumbar surgery. The open surgery group had significantly higher incidence of DT than the MIS group (15.9% versus 6.4%, p<0.05). Overall, the incidence of DT was less in males (10.9%) compared with females (14.6%), but this difference was statistically insignificant (p>0.05). The inter-group comparison was also not significant (p>0.05) (Table 2).
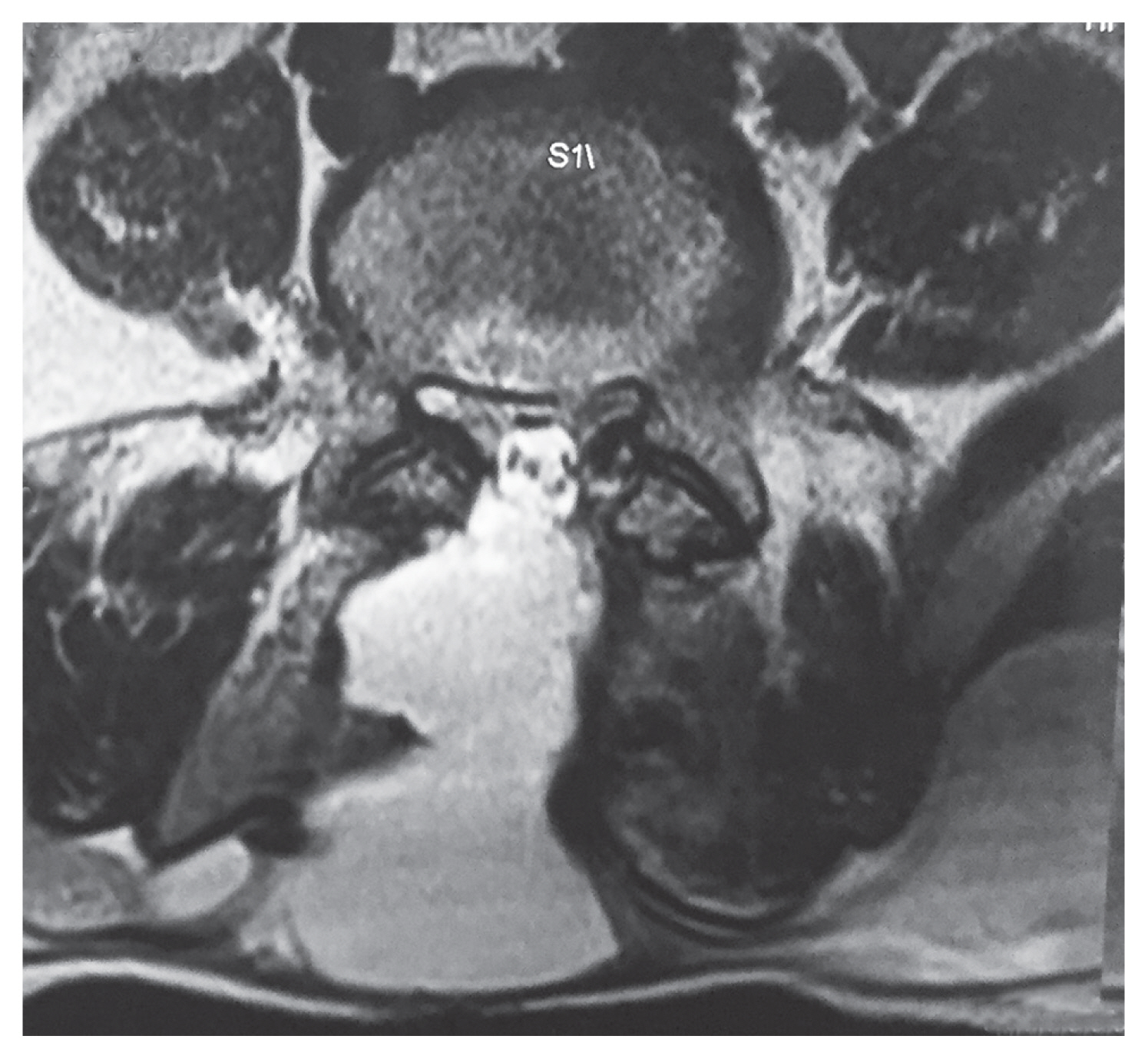
Postoperative magnetic resonance imaging showing pseudo-meningocele formation after open lumbar decompression.

Intraoperative picture showing revision suturing for a patient of persistent dural leak with pseudo-meningocele formation.
The risk factors for DT in both groups were evaluated. The distribution of risk factors, such as high BMI (≥25.0 kg/m2), comorbidities, addiction (smoking, alcohol), and history of previous surgery, was comparable between the two groups (Table 1). The incidence of DT was significantly high in patients with high BMI, patients with diabetes mellitus, and patients who underwent revision surgery (p<0.05), regardless of the surgical approach (Tables 2, 3). No other risk factors had a statistically significant effect on the incidence of DT.
Regarding the incidence of DT based on the type of surgery, the incidence of DT was significantly less for MIS discectomy than for open surgery (4.2% versus 19.4%, p=0.028). For revision surgery, the DT was significantly less in the MIS group than in the open surgery group (5.9% versus 40.0%, p=0.029). For TLIF and decompression surgery (laminectomy/laminotomy), the incidence of DT was similar between the open surgery and MIS groups, with no statistically significant difference (p>0.05) (Table 2).
Regarding return to work, patients from the open surgery group were declared fit to work at 6.8±1.1 weeks after the surgery, whereas the patients from the MIS group were declared fit to work at 4.5±0.7 weeks after the surgery (Table 2). This difference was statistically significant (p<0.001), suggesting that the MIS approach enabled an earlier return to work, thereby indirectly reducing the economic impact of the surgery. Among patients suffering from a DT after open surgery, the mean return to work was at 8.4±1.1 weeks postoperatively. In comparison, those complicated by a durotomy after MIS returned to work after 5.5±0.9 weeks. This difference was also statistically significant (p<0.001) (Table 2), suggesting that even after an accidental durotomy, the patients who were operated on using the MIS approach were able to return to work earlier than those operated on using an open surgery approach without a durotomy.
Discussion
Among 420 prospective follow-up cases of degenerative lumbar spine surgery, 12.4% had an unintended durotomy in our study. The incidence of DT varies between 0.3% and 35% in the literature [1–6], depending on the type of surgery and the approach. For prospective studies, the reported incidence of DT ranges between 3% and 20% [11]. In their systematic review, Ghobrial et al. [11] found that the incidence of DT was twice as high in prospective studies (9.6%) compared with retrospective studies (4.3%). In our study, the incidence of DT was significantly less in the MIS group than in the open surgery group (6.4% versus 15.9%). While there are many meta-analyses and literature reviews on incidental durotomy in open surgeries, most studies on MIS have relatively small prospective or retrospective cohorts [11–16]. In the absence of matched cohort studies, it is difficult to compare the incidence of DT in open versus MIS groups. Even after a systematic review of literature, we concluded that no significant difference exists in the incidence of DT among the two groups. The lack of background patient characteristics (i.e., BMI) and a small data pool have been cited as limiting factors in the identification of more meaningful comparative data while comparing the open surgery and MIS groups [11]. Wong et al. [17] concluded that patients who underwent open spine surgery were 2 times more likely to have a CSF leak. In their study, the incidence of DT was significantly less in the MIS group than in the open surgery group (4.7% versus 9%), which was consistent with our study results [17].
Revision surgery, diabetes mellitus, high BMI, female sex, and increased age have all been documented as risk factors of DT [18–20]. In our study, high BMI, diabetes mellitus, and revision surgery were identified as independent risk factors, regardless of the approach (Tables 2, 3). In our study, the age distribution was comparable; this was also reflected in the incidence of DT, which was comparable across the different age groups. Based on our findings, a higher age does not significantly affect the chances of durotomy (Tables 1, 2).
The overall incidence of DT was less in MIS, regardless of the type of surgery. For discectomy cases, the incidence of DT was significantly less in the MIS group than in the open surgery group (4.2% versus 19.4%); a similar pattern was observed in revision surgeries. In decompression surgery (laminectomy/laminotomy) and TLIF, the incidence of DT was similar between surgical approaches without any significant difference (p>0.05). The tubular system allows a surgeon to have a great amount of mobility in approaching the disc fragment. Surgeons can specifically target the pathological disc fragment without needing significant tissue or bone dissection. The MIS approach during discectomy mainly involves flavectomy or a small laminotomy, wherein a small amount of ligamentum flavum or lamina is removed to approach the disc. In the open surgery approach, the amount of laminectomy or flavectomy is comparatively higher. This may explain why the MIS approach had a lower risk of DT in cases of discectomy, as the additional and extensive dissection needed for the open surgery approach can lead to a higher probability of DT, especially in cases where significant compression is present. Furthermore, although the narrow corridor provided by the MIS approach may make the procedure challenging, any potential tears are usually tiny due to the minimal tissue retraction. In turn, this protects against the formation of a pseudomeningocele or a cerebrospinal fistula [21]. Similarly, in revision surgery, the tubular approach also allows the surgeon to skip the midline scar tissue and fibrosis, resulting in a smaller chance of incidental DT. In TLIF and decompression surgery, the extent of laminectomy or flavectomy is slightly less compared with open surgery. Good decompression plays an important role in these surgeries, whereas the basic principles of surgery remain unchanged. Thus, the risk of DT is not significantly different between TLIF and decompression surgery regardless of the approach. The available literature comparing the different types of surgery is currently limited [11,14,22]. Most studies mention the risk of DT only in one specific type of surgery, either open surgery or MIS. Despite a review of literature comparing the different studies, no significant difference in the risk of DT was found between the two approaches [12,13,15,16]. We feel that the lack of a matched cohort in the current literature makes it difficult to compare the incidence of DT among different surgical techniques.
In our study, four patients in the open surgery group underwent revision surgery due to persistent CSF leak and pseudomeningocele formation, whereas two cases presented with delayed dural leak 1 month following open lumbar decompression. We believe that the loss of posterior elements and paraspinal muscle cover increases the risk of revision surgery and delayed dural leaks in open surgery (Figs. 1, 2). In MIS, the oblique corridor between the multifidus and longissimus preserves the soft tissue elements, providing a natural barrier against dural leak. These further complications are prevented in MIS as it has less dead space (Figs. 3, 4). In all cases of DT in open surgery, primary repair was attempted, whereas MIS cases were managed using an EVICEL Fibrin Sealant and a layer of fat pad. However, the ideal method of dural repair remains a matter of debate. Primary repair remains the most accepted technique, but several studies have found no difference in patient outcomes or complications among the techniques of dural closure. Kamenova et al. [23] found no difference in the revision rates at 6 weeks among the dural closure techniques of dural suture, patch only (TachoSil and/or muscle and/or fat), and dural suture with patch. In our study, none of the patients underwent revision surgery in the MIS group, and no primary repair was attempted in this group.

Postoperative magnetic resonance imaging in a case of dural tear following minimally invasive spine surgery tubular decompression.
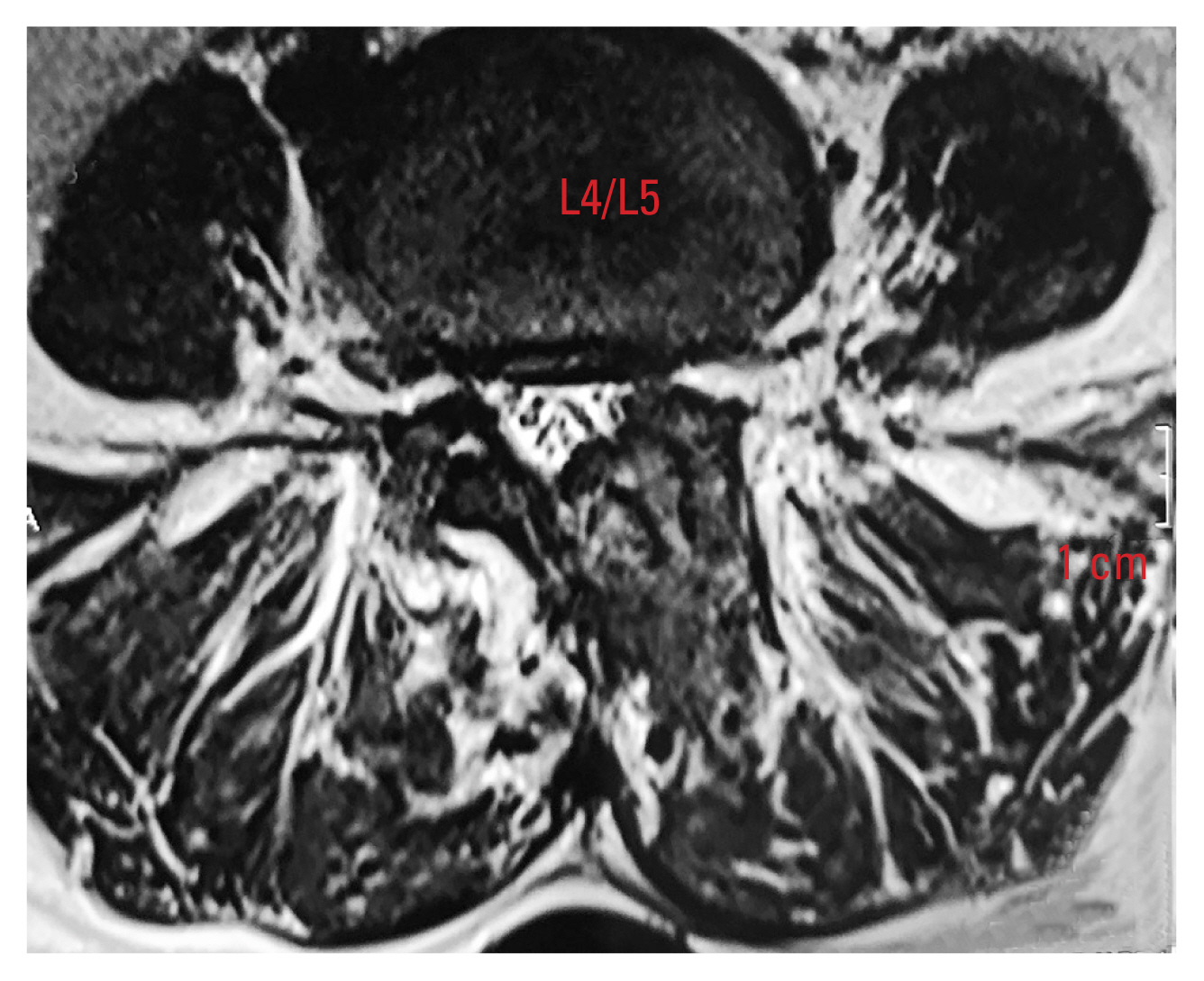
Follow-up magnetic resonance imaging in a case of dural tear following minimally invasive spine surgery tubular decompression.
There have been various observations regarding the return to work. Silva et al. [24] reported that 68.4% of their patients did not return to work. Adogwa et al. [25] found that MIS and open surgery patients returned to work at a median of 8.5 and 17.1 weeks, respectively. Similarly, Parker et al. [26] observed that MIS and open surgery patients returned to work at 8.3 and 16.3 weeks, respectively. Although we reported an earlier return to work compared with all these studies, our findings were nevertheless in agreement with those of previous studies in that MIS indeed enables a quicker work resumption.
The limitations of our study include its nonrandomized nature and being a single-center study. Being a nonrandomized study, our study may have bias in the selection of one approach over the other. However, all procedures were performed by the same spine team, thus minimizing the selection bias. There may have been a bias regarding the learning curve for MIS, although we excluded MIS cases in the first 6 months to avoid this. The surgical approach was decided by the surgeon after consultation with the patients. We excluded complex deformities and >3 level surgeries as they are more likely to be chosen for an open surgery approach. Most decompression surgeries were performed via the open surgery approach in our series, although we found no significant differences in the rates of DT in the decompression surgery regardless of the approach. A future randomized study will definitely contribute much to the literature.
Conclusions
MIS is associated with a significantly lower incidence of DT compared with open surgery among patients with degenerative lumbar pathology. Patients managed using the MIS approach were also able to resume their work earlier than those managed using the open surgery approach. Even in the presence of an incidental DT, patients treated via the MIS had better postoperative outcomes with an earlier return to work compared with those managed via open surgery.
Notes
Conflict of Interest
No potential conflict of interest relevant to this article was reported.
Author Contributions
Study design: Ayush Sharma, Akash Shakya, Vijay Singh; data collection: Priyank Deepak, Nilesh Mangale, Ajay Jaiswal, Nandan Marathe; data analysis: Akash Shakya; manuscript writing: Akash Shakya, Priyank Deepak; proof-reading: Akash Shakya; and final approval of manuscript: all authors.