2. Mac-Thiong JM, Roussouly P, Berthonnaud E, Guigui P. Age- and sex-related variations in sagittal sacropelvic morphology and balance in asymptomatic adults. Eur Spine J 2011;20(Suppl 5): 572–7.


4. Boulay C, Tardieu C, Hecquet J, et al. Sagittal alignment of spine and pelvis regulated by pelvic incidence: standard values and prediction of lordosis. Eur Spine J 2006;15:415–22.


5. Mac-Thiong JM, Berthonnaud E, Dimar JR 2nd, Betz RR, Labelle H. Sagittal alignment of the spine and pelvis during growth. Spine (Phila Pa 1976) 2004;29:1642–7.


7. Garagiola DM, Tarver RD, Gibson L, Rogers RE, Wass JL. Anatomic changes in the pelvis after uncomplicated vaginal delivery: a CT study on 14 women. AJR Am J Roentgenol 1989;153:1239–41.


8. Samuel CS, Butkus A, Coghlan JP, Bateman JF. The effect of relaxin on collagen metabolism in the nonpregnant rat pubic symphysis: the influence of estrogen and progesterone in regulating relaxin activity. Endocrinology 1996;137:3884–90.


10. Whitcome KK, Shapiro LJ, Lieberman DE. Fetal load and the evolution of lumbar lordosis in bipedal hominins. Nature 2007;450:1075–8.


12. Bailey JF, Sparrey CJ, Williams FM, Curran PF, Lotz JC, Kramer PA. The effect of parity on age-related degenerative changes in sagittal balance. Spine (Phila Pa 1976) 2020;45:E210–6.


13. Arima H, Dimar JR 2nd, Glassman SD, et al. Differences in lumbar and pelvic parameters among African American, Caucasian and Asian populations. Eur Spine J 2018;27:2990–8.


14. Yamato Y, Sato Y, Togawa D, et al. Differences in the geometrical spinal shape in the sagittal plane according to age and magnitude of pelvic incidence in healthy elderly individuals. J Orthop Sci 2020;25:557–64.


15. Oe S, Togawa D, Nakai K, et al. The influence of age and sex on cervical spinal alignment among volunteers aged over 50. Spine (Phila Pa 1976) 2015;40:1487–94.


16. Yoshida G, Yasuda T, Togawa D, et al. Craniopelvic alignment in elderly asymptomatic individuals: analysis of 671 cranial centers of gravity. Spine (Phila Pa 1976) 2014;39:1121–7.

17. Ushirozako H, Yoshida G, Hasegawa T, et al. Impact of shift to the concave side of the C7-center sacral vertical line on de novo degenerative lumbar scoliosis progression in elderly volunteers. J Orthop Sci 2020;25:82–8.


18. Mihara Y, Togawa D, Hasegawa T, et al. Lumbar Retrolisthesis compensates spinal kyphosis. Spine Deform 2019;7:602–9.


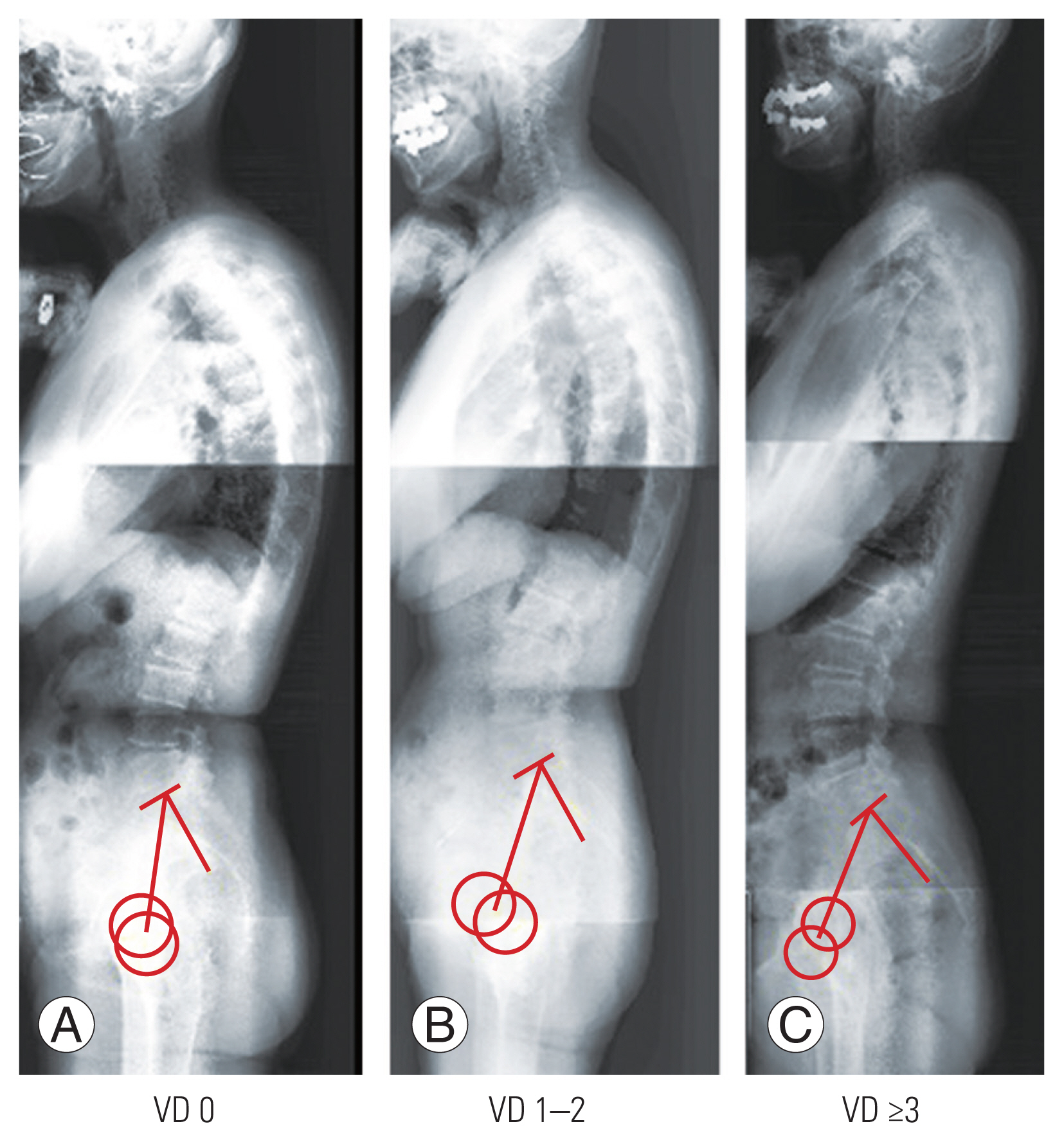
19. Genant HK, Wu CY, van Kuijk C, Nevitt MC. Vertebral fracture assessment using a semiquantitative technique. J Bone Miner Res 1993;8:1137–48.


20. Faro FD, Marks MC, Pawelek J, Newton PO. Evaluation of a functional position for lateral radiograph acquisition in adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 2004;29:2284–9.


21. Banno T, Hasegawa T, Yamato Y, et al. T1 pelvic angle is a useful parameter for postoperative evaluation in adult spinal deformity patients. Spine (Phila Pa 1976) 2016;41:1641–8.


23. Borell U, Fernstrom I. The movements at the sacro-iliac joints and their importance to changes in the pelvic dimensions during parturtion. Acta Obstet Gynecol Scand 1957;36:42–57.


24. Roberts CL, Nippita TA. International caesarean section rates: the rising tide. Lancet Glob Health 2015;3:e241–2.


26. Weisl H. The articular surfaces of the sacro-iliac joint and their relation to the movements of the sacrum. Acta Anat (Basel) 1954;22:1–14.