|
 |
- Search
| Asian Spine J > Volume 10(4); 2016 > Article |
Abstract
Purpose
This study aims to investigate the accuracy of the oblique fluoroscopic view, based on preoperative computed tomography (CT) images for accurate placement of lumbosacral percutaneous pedicle screws (PPS).
Overview of Literature
Although PPS misplacement has been reported as one of the main complications in minimally invasive spine surgery, there is no comparative data on the misplacement rate among different fluoroscopic techniques, or comparing such techniques with open procedures.
Methods
We retrospectively selected 230 consecutive patients who underwent posterior spinal fusion with a pedicle screw construct for degenerative lumbar disease, and divided them into 3 groups, those who had undergone: minimally invasive percutaneous procedure using biplane (lateral and anterior-posterior views using a single C-arm) fluoroscope views (group M-1), minimally invasive percutaneous procedure using the oblique fluoroscopic view based on preoperative CT (group M-2), and conventional open procedure using a lateral fluoroscopic view (group O: controls). The relative position of the screw to the pedicle was graded for the pedicle breach as no breach, <2 mm, 2ŌĆō4 mm, or >4 mm. Inaccuracy was calculated and assessed according to the spinal level, direction and neurological deficit. Inter-group radiation exposure was estimated using fluoroscopy time.
Results
Inaccuracy involved an incline toward L5, causing medial or lateral perforation of pedicles in group M-1, but it was distributed relatively equally throughout multiple levels in groups M-2 and controls. The mean fluoroscopy time/case ranged from 1.6 to 3.9 minutes.
Conclusions
Minimally invasive lumbosacral PPS placement using the conventional fluoroscopic technique carries an increased risk of inaccurate screw placement and resultant neurological deficits, compared with that of the open procedure. Inaccuracy tended to be distributed between medial and lateral perforations of the L5 pedicle, as a result of pedicle morphology and the PPS pathway. Oblique fluoroscopic views, based on CT measurement, may allow accurate PPS insertion with a shorter fluoroscopy time.
Percutaneous pedicle screw (PPS) placement is gradually being adopted for lumbar and thoracic spine surgeries, requiring minimally invasive fixation [123]. Most studies are designed to emphasize the favorable advantages of minimally invasive surgery (MIS), such as lowered invasiveness for posterior spinal muscles, and shorter hospital stay and clinical outcomes similar to those of the conventional open procedure. In contrast, PPS placement is seemingly more technically demanding because of a lower number of landmarks that can be palpitated during surgery, which can lead to potentially significant radiation exposure and inaccurate screw placement, causing potential neurological deficits. Reports have indicated 4.7%ŌĆō23% inaccuracy in PPS placement, and many of these inaccurate placements resulted in pathological consequences after MIS [4567]. Some authors reported the accuracy of percutaneous pedicle screws (PS) placement using computer-assisted navigation systems and complex guidance devices, resulting in clinical outcomes similar to those of conventional open procedures [78910]. However, these systems and devices have not achieved widespread use because of the associated increased costs, longer set-up times, and technical difficulty.
Only a few studies have described the methods for accurate insertion percutaneous lumbar PSs using fluoroscopy, similar to conventional open procedures [1112]. Furthermore, no studies have compared the differences in mechanism and trends in resultant inaccuracies between open procedures and MIS, or the difference in radiation exposure in MIS among different fluoroscopic techniques. This study compared the tendency of screw malposition during the percutaneous procedure and the conventional open procedure, and investigated the efficacy of the oblique fluoroscopic view based on simple computed tomography (CT) measurements for accurate placement of lumbosacral PPS and reducing radiation exposure.
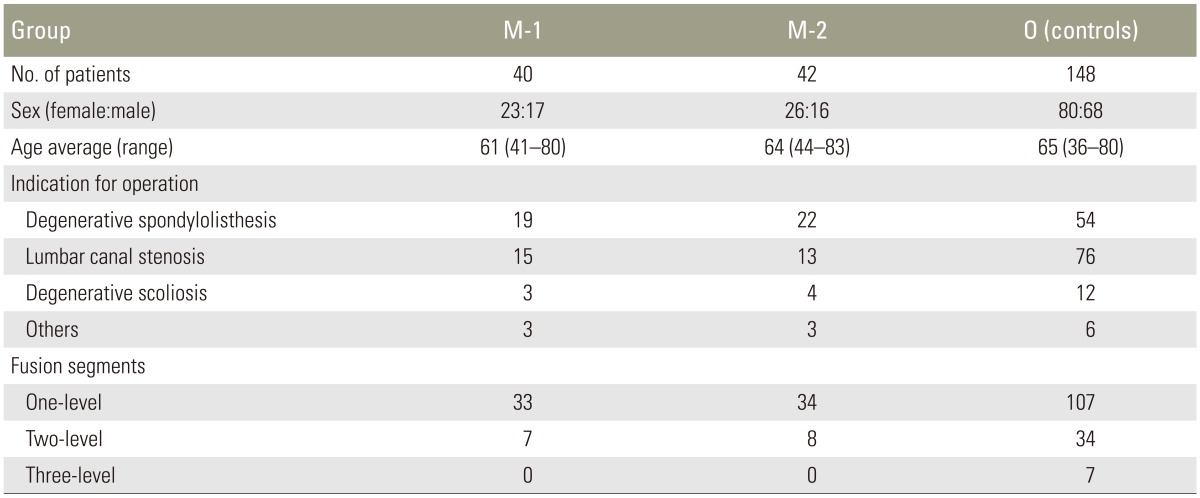
After obtaining Institutional Review Board approval, we conducted a retrospective study involving 266 consecutive patients who underwent posterior (PLIF [13])/transpedicular lumbar interbody fusion (TLIF [14]) and placement of PS constructs for lumbar disorders between January 2008 and June 2014 in the first author-associated 2 hospitals (Hamamatsu Medical Center and Konan Kosei Spine Center). Subsequently, 36 patients were excluded on the grounds of previous lumbar surgery. The remaining 230 patients were divided into group M-1, having undergone a minimally invasive percutaneous procedure using bi-planer (lateral and anterior-posterior [AP]) fluoroscopic view; group M-2, having undergone a minimally invasive percutaneous procedure using the oblique fluoroscopic view based on simple CT measurements, and group O (controls), having undergone a conventional open procedure using lateral fluoroscopic view. The patient characteristics and procedure data of these groups are listed in Table 1.
Lumbar interbody fusion and PS placement was determined from lower back pain, the patients' predominant complaint, with varying degrees of radiating pain, neurological complaints, or a combination of these. Selection criteria for open procedure or MIS depended upon the availability of the procedure at the time of surgery. MIS was implemented later than open procedure in the series, because of its popularity at the time, but the indications for both surgeries were the same. MIS subgroups (M-1 and M-2) were almost randomly chosen because that were handled by one or another fashion in turn for each hospital. In the M-1 and M-2 groups, pedicle screw was inserted percutaneously, rather than through a paramedian mini-open technique.
When preparing for the percutaneous procedures, the operation table was adjusted to vertically position the fusion segment, and a true AP view was confirmed by centering the spinous process between the pedicles.
Percutaneous PS placement was as follows: (1) Pedicles were introduced with trocar needles positioned at the junction of the pedicle and the posterior cortex of the vertebral body using biplane (lateral and AP views using a single C-arm) fluoroscopic views (group M-1) or an oblique fluoroscopic view (group M-2). (2) After the needle was within the pedicle, stylets were removed and guidewires were inserted. Soft tissue dilators were used to create paths for the taps and screws. (3) Cannulated screws were placed over the guidewires. Rods were inserted percutaneously in order to minimize soft tissue trauma. (4) Interbody implants were placed, as described by Schwender et al. [15] as MIS-TLIFs, using tubular retractors. In group M-2, obliquity of fluoroscopy was chosen on the basis of the preoperative CTs. The insertion angle from the axial plane was equal to the obliquity of fluoroscopy and was measured by subtracting the angle between the line passing through the centre of the pedicle and the sagittal line in axial CTs. This angle was measured for each vertebra having an inserted PS. A representative case is shown in Figs. 1 and 2. The inserting screw length and diameter were measured before surgery using axial CTs. We used 6 different percutaneous systems: Pathfinder (MDM, Inc.; a division of Abbott Spine, Austin, TX, USA); Sextant (Medtronic Sofamor Danek, Memphis, TN, USA); Viper (DePuy Spine, a division of Johnson & Johnson, Arlington, TX, USA); Spirit (Synthes, West Chester, PA, USA); Mantis (Stryker, Kalamazoo, MI, USA); and Ilico SE (Alphatec Spine, Carlsbad, CA, USA), however, all PSs were of similar length and diameter, which was 40ŌĆō45 mm long with a 6.0ŌĆō6.5-mm diameter.
Open PS placement was performed as described by Michele and Krueger [16] using the midline open approach. After exposing the dorsal pedicle entry point or transverse process junction, lateral fluoroscopy was used during the insertion procedure. In all conventional open procedures, screws were placed between decompression and interbody implant placement times (PLIF or TLIF) with visualization of the lateral aspects of the spinal canal. LEGACY 5.5 Spinal System (Medtronic Sofamor Danek, Memphis, TN, USA) was used for all group O patients. All inserted screws were 40ŌĆō45 mm long, with a 6.5-mm diameter.
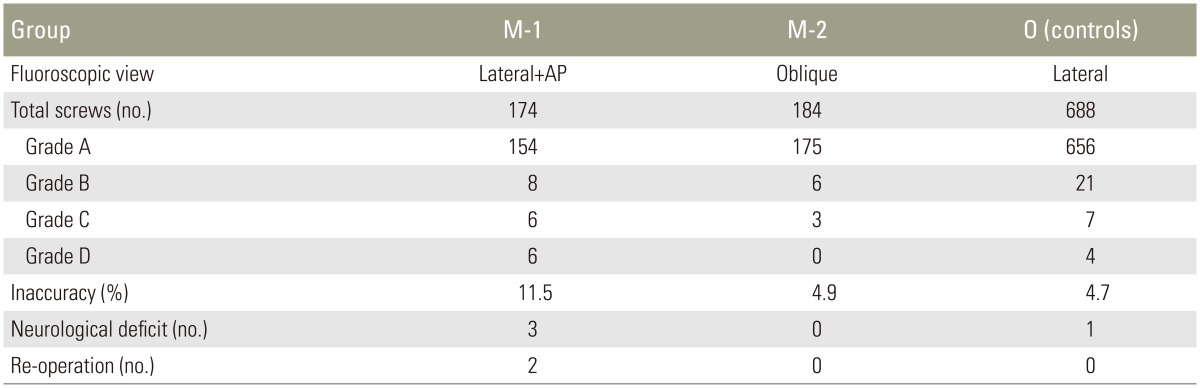
Preoperative CTs were evaluated in all patients, even those undergoing the open procedure. They were mainly used to achieve a precise diagnosis, including any degenerative changes to the facet joint, spondylolisthesis, anomalies or distorted anatomy. Postoperative fine-cut (2.0-mm slices) CTs were also obtained for all patients. The accuracy of PS placement into the medial/lateral pedicle walls was evaluated on axial CTs, whereas the superior/inferior pedicle wall screw location was examined on reconstructed sagittal or coronal CTs. Assessments were performed by an independent spinal surgeon. The relative positions of the screws to the pedicles were assessed and classified as A, completely within the pedicle; B, pedicle wall breach <2 mm; C, pedicle wall breach of 2ŌĆō4 mm; or D, pedicle wall breach >4 mm (Fig. 3). The borderline positions were automatically downgraded (i.e., A-to-B, B-to-C, etc.). Inaccurate PS placement is considered as a potential risk factor for neurovascular injury; a measure of that risk was calculated as follows: inaccurate PS placement=(number of screws, grades B+C+D)/(number of screws, grades A+B+C+D)├Ś100.
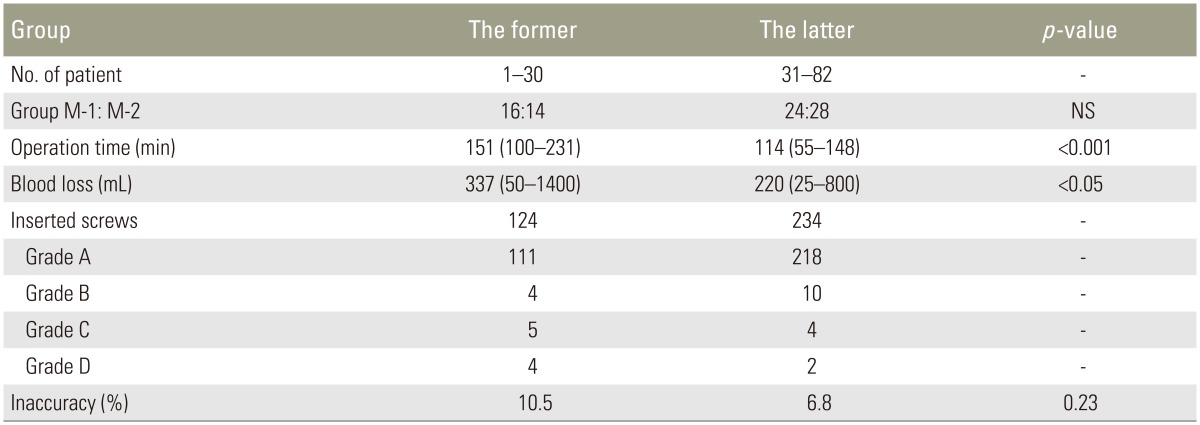
All percutaneous procedures (groups M-1 and M-2) were performed by 1 surgeon. Any new skills required for a surgery, such as for MIS-TLIFs, have resulted in a "learning curve" for the procedure. We used the operative time, blood loss, and accuracy of screw placement as objective measures for surgeon experience in the percutaneous procedure-related learning curves. These parameters were evaluated and divided into 2 groups of former and latter periods at the time of surgery to make allowances for the surgeon's experience. Patients were divided into former patients, patients 1ŌĆō30; and latter patients, patients 31ŌĆō82.
A fluoroscope with a 19-inch image intensifier (Siremobil Compact L, Siemens, Belgium) was used; both one-shot and automatic-continuous modes were used at the right moment to minimize radiation exposure and to achieve consistent image quality. We extrapolated the approximate radiation exposure from the fluoroscopic time, which was recorded during all procedures, including PS insertion and interbody fusion.
In total, 1046 PSs were placed in 230 consecutive patients. Groups M-1, M-2 and controls (group O) comprised 40, 42 and 148 patients with 174, 184 and 688 inserted screws, respectively. Malposition rates of MIS (groups M-1 plus M-2) and controls were 8.1% and 4.7%, respectively. The degree of perforation in controls gradually decreased as follows: grades B, C, and D were 21, 7, and 4, respectively. In contrast, the degree of perforation of the pedicle in group M-1 were as follows: grades B, C, and D were 8, 6, and 6 screws, respectively, and the inaccuracy was 11.5%. Group M-2 used the oblique view of fluoroscopy, and the degree of perforation of the pedicle gradually decreased as follows: grades B, C, and D were 6, 3, and 0, respectively.
A statistically significant difference was observed in accuracy between M-1 and controls, and between M-1 and M-2. Three of 6 grade Ds incorrectly placed PSs in group M-1 caused a neurological deficit; they were re-inserted during another surgery (Fig. 3). No anterior vertebral perforation was observed for any screw in the control or MIS group. A summary of the accuracy data comparisons between the groups is presented in Table 2. The level and direction of inaccuracies are listed in Table 3. Malpositioned screws were inclined towards L5 in group M-1, whereas they showed relatively equal distribution throughout the multi-levels in M-2 and controls. Furthermore, in group M-1, inaccuracy tended to gather at a horizontal plane as medial or lateral perforations of the pedicle.
In total, 358 percutaneous PSs were placed in 82 patients who underwent MIS-TLIF. The mean operation time in the former (patients 1ŌĆō30), and latter (patients 31ŌĆō82) groups was 151 minutes (range, 100ŌĆō231 minutes) and 114 minutes (range, 55ŌĆō148 minutes), respectively. The latter had a significantly shorter operation time than the former (p<0.001). The mean blood loss in the former and latter groups was 337 mL (range, 10ŌĆō1,400 mL) and 220 mL (range, 66ŌĆō800 mL), respectively. The latter had significantly lower blood loss than the former (p<0.05); however, there was no significant difference in accuracy between the former and the latter groups (p>0.05) (Table 4).
Mean fluoroscopy time/case in groups M-1, M-2 and controls was 3.9 minutes (range, 1.6ŌĆō7.8 minutes), 1.8 minutes (range, 1.2ŌĆō4.4 minutes), and 1.6 minutes (range, 1.0ŌĆō5.8 minutes), respectively, with a statistically significant difference between group M-1 and controls (p<0.05), and between groups M-1 and M-2 (p<0.05).
The first percutaneous placement PS, described by Magerl [17], was subsequently used for only temporary external fixation, but was further developed for percutaneous internal fixation. Since then, several studies have described percutaneous techniques for posterior lumbar fusion to avoid iatrogenic injury to the dorsal musculoligamentous unit [123]. However, the limitations of MIS using percutaneous PSs include the learning curve required, exposure to radiation, and implant-associated complications. In particular, PS malpositioning may cause neurovascular injury, pedicle fracture, pseudoarthosis, and other problems. In MIS, surgeons lack the ability to visualize and palpate bony landmarks and the decompressed spinal canal itself; they must therefore rely heavily on fluoroscopic assistance. With the absence of true anatomical vision, the incidence of pedicle breach would be higher than in conventional open procedures. Few studies have reported on the differences in accuracy of PS placement between open procedures and MIS using conventional fluoroscopy.
This study reported that the open procedure was accurate in 95.3% of 688 screws, similar to previous studies. In contrast, MIS was accurate in 91.9% of cases, and the malpositioned screws in group M-1 tended to be placed far from the pedicle. In this study, there were no significant differences in complication rates, including infection, screw pull-out or pseudoarthrosis, except for the neurological deficits between group M-1 and M-2. Furthermore total OP time was almost the same for both procedures. However, the inaccuracy and radiation exposure in group M-2 were less than that observed in group M-1. We suspected that the high inaccuracy of percutaneous screw placement may be because of the entry points and pathways used for this procedure are different from those in the open procedure, and because the pedicle morphology of L5 is quite varied [1819]. The entry point of the percutaneous lumbar PS is more lateral than that of the open procedure, and its pathway is steep on the axial plane. The axis of the lumbar pedicles on the sagittal midline plane varies with the spinal level; the angle of the L5 pedicle axis is the largest. This steep angle makes it difficult to insert PSs accurately using the conventional fluoroscopic technique. Furthermore, the highest pedicle breach rate in L5 is considered to be due to the different shapes of pedicle, depending on the height [20]. L5 pedicular width and direction in the upper and lower parts are different. In the lower parts, L5 pedicle has a narrow shape and more convergent angle than the upper part. Subsequently, if the L5 PS is introduced at the same convergent angle as the higher part, it may cause lateral recess perforation in the lower part. The same phenomenon may occur at the S1 level.
Controversy exists over what is the best technique to achieve accurate percutaneous PS insertion using the conventional fluoroscopic technique. One example is the Magerl technique, termed the owl's-eye technique; another is a modified technique using AP and lateral fluoroscopic views. In a cadaveric study, Wiesner et al. [21] reported that no significant difference exists between the 2 techniques, but they found a higher misplacement rate in the upper lumbar spine using the Magerl technique. They also reported a 6.6% inaccuracy with 2 nerve injuries (L4 and L5), and that S1 showed the highest malposition rate (12%) using the modified technique in an in vivo lumbar spine [22]. Power et al. [12] recommended the owl's-eye technique for sighting in line with the pedicle. This technique helps surgeons to be constantly aware of the medial pedicle wall and, when performing percutaneous screw placement at S-1, without being readily aware of the initial entry point. In this previous research, they explained that connecting the medial aspect of the pedicle with the levels above helps to identify the medial aspect of S-1. Idler et al. [13] also recommended the owl's-eye technique using a novel guidance technology; they noted that the true pedicle axis enables the cephalad facet complex to be clearly visualized and avoided.
Crucially, however, the owl's eye technique requires manoeuvring by a skilful operator to achieve a clear radiographic demonstration. In this study, we used the oblique view of fluoroscopy, an angle that was easily adjusted on simple preoperative CTs. Consequently, it is easy to handle the fluoroscope, even if the nurse or resident using it chooses obliquity. Furthermore, this technique allows reduction of inadvertent labour hours to adjust the obliquity of the fluoroscope during surgery as well as radiation exposure, because the angle is measured on the preoperative CTs. Exact obliquity is beneficial for preventing adjacent joint disorder, because the facet joint is clearly visible. Most importantly, this is the only fluoroscopic technique to safely and accurately insert percutaneous PSs without the aid of other devices.
This study has several limitations; its retrospective design and the accuracy of percutaneous PS placement depends upon a learning curve. In general, the surgeon's experience improves the outcome of various procedures. The association between higher volumes and better outcomes has been established for some spinal surgeries, such as cervical PS placement, and lumbar endoscopic discectomy [232425]. The same holds true for MIS-TLIF using percutaneous PS placement. Operating time and blood loss were decreased as surgeons overcame the learning curve for the technical difficulty in this series. However, the accuracy of PS placement using the percutaneous procedure did not clearly depend on the surgeon's experience, because of the pedicle morphology and the optical illusion of the PS pathway using AP and lateral fluoroscopic views. Other limitations included the use of different types of implants, the rate of screw placement at the S1 level being relatively low, data on fluoroscopy time did not accurately reflecting the true radiation exposure because the time estimated included the time of interbody fusion, and the amount of radiation exposure was different from the incidence angle of the fluoroscope.
Many complicated devices and computed navigation systems for accurately inserting percutaneous PSs in MIS are available and widespread use is much expected in the near future. However, the best way to safely and accurately place percutaneous PSs is to study the multitude of clinical experiences and anatomical knowledge of open spinal procedures. We consider that the conventional oblique fluoroscopic technique is freely available and it that can be easily introduced and performed, even by surgeons with limited experience. Acceptable results may be achieved even by spinal surgeons who are accustomed to the open procedure with the conventional fluoroscopic technique.
The placement of percutaneous lumbosacral PSs using the conventional fluoroscopic technique carries an increased risk of inaccurate screw placement and resultant neurological deficits, compared with the conventional open procedure. Inaccuracy in our study tended to be distributed between the medial and lateral perforations of the L5 pedicle because of pedicle morphology and the percutaneous PS pathway. Besides reducing radiation exposure, being easily introduced without other devices and manoeuvrable even by inexperienced surgeons, the oblique fluoroscopic technique is advantageous because it is based on simple CT measurements that can improve accuracy and safety in percutaneous PS placement.
Notes
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
References
1. Foley KT, Gupta SK. Percutaneous pedicle screw fixation of the lumbar spine: preliminary clinical results. J Neurosurg 2002 97(1 Suppl): 7ŌĆō12. PMID: 12120655.


2. Ringel F, Stoffel M, Stuer C, Meyer B. Minimally invasive transmuscular pedicle screw fixation of the thoracic and lumbar spine. Neurosurgery 2006 59(4 Suppl 2): ONS361ŌĆōONS366. PMID: 17041505.



3. Harris EB, Massey P, Lawrence J, Rihn J, Vaccaro A, Anderson DG. Percutaneous techniques for minimally invasive posterior lumbar fusion. Neurosurg Focus 2008 25:E12PMID: 18673041.

4. Nakashima H, Sato K, Ando T, Inoh H, Nakamura H. Comparison of the percutaneous screw placement precision of isocentric C-arm 3-dimensional fluoroscopy-navigated pedicle screw implantation and conventional fluoroscopy method with minimally invasive surgery. J Spinal Disord Tech 2009 22:468ŌĆō472. PMID: 20075808.


5. Wood MJ, Mannion RJ. Improving accuracy and reducing radiation exposure in minimally invasive lumbar interbody fusion. J Neurosurg Spine 2010 12:533ŌĆō539. PMID: 20433301.


6. Kim MC, Chung HT, Cho JL, Kim DJ, Chung NS. Factors affecting the accurate placement of percutaneous pedicle screws during minimally invasive transforaminal lumbar interbody fusion. Eur Spine J 2011 20:1635ŌĆō1643. PMID: 21720727.



7. Ravi B, Zahrai A, Rampersaud R. Clinical accuracy of computer-assisted two-dimensional fluoroscopy for the percutaneous placement of lumbosacral pedicle screws. Spine (Phila Pa 1976) 2011 36:84ŌĆō91. PMID: 20595927.


8. Holly LT, Foley KT. Three-dimensional fluoroscopy-guided percutaneous thoracolumbar pedicle screw placement: technical note. J Neurosurg 2003 99(3 Suppl): 324ŌĆō329. PMID: 14563154.


9. Fraser J, Gebhard H, Irie D, Parikh K, Hartl R. Iso-C/3-dimensional neuronavigation versus conventional fluoroscopy for minimally invasive pedicle screw placement in lumbar fusion. Minim Invasive Neurosurg 2010 53:184ŌĆō190. PMID: 21140333.



10. von Jako R, Finn MA, Yonemura KS, et al. Minimally invasive percutaneous transpedicular screw fixation: increased accuracy and reduced radiation exposure by means of a novel electromagnetic navigation system. Acta Neurochir (Wien) 2011 153:589ŌĆō596. PMID: 21153669.


11. Idler C, Rolfe KW, Gorek JE. Accuracy of percutaneous lumbar pedicle screw placement using the oblique or "owl's-eye" view and novel guidance technology. J Neurosurg Spine 2010 13:509ŌĆō515. PMID: 20887149.


12. Powers CJ, Podichetty VK, Isaacs RE. Placement of percutaneous pedicle screws without imaging guidance. Neurosurg Focus 2006 20:E3PMID: 16599419.

13. Cloward RB. The treatment of ruptured lumbar intervertebral discs by vertebral body fusion. I. Indications, operative technique, after care. J Neurosurg 1953 10:154ŌĆō168. PMID: 13035484.


14. Harms JG, Jeszenszky D. The unilateral transforaminal approach for posterior lumbar interbody fusion. Orthop Traumatol 1998 6:88ŌĆō99.
15. Schwender JD, Holly LT, Rouben DP, Foley KT. Minimally invasive transforaminal lumbar interbody fusion (TLIF): technical feasibility and initial results. J Spinal Disord Tech 2005 18(Suppl): S1ŌĆōS6. PMID: 15699793.


16. Michele AA, Krueger FJ. Surgical approach to the vertebral body. J Bone Joint Surg Am 1949 31:873ŌĆō878. PMID: 18142931.

17. Magerl FP. Stabilization of the lower thoracic and lumbar spine with external skeletal fixation. Clin Orthop Relat Res 1984 (189): 125ŌĆō141. PMID: 6478690.


18. Olsewski JM, Simmons EH, Kallen FC, Mendel FC, Severin CM, Berens DL. Morphometry of the lumbar spine: anatomical perspectives related to transpedicular fixation. J Bone Joint Surg Am 1990 72:541ŌĆō549. PMID: 2139030.


19. Mitra SR, Datir SP, Jadhav SO. Morphometric study of the lumbar pedicle in the Indian population as related to pedicular screw fixation. Spine (Phila Pa 1976) 2002 27:453ŌĆō459. PMID: 11880829.


20. Alfonso M, Palacio P, Bastarrika G, Villas C. Does the shape of the L5 vertebral body depend on the height of CT slices in the pedicle? Evaluation of the shape of the L5 vertebral body with a multicut CT scan. Spine (Phila Pa 1976) 2008 33:E1ŌĆōE5. PMID: 18165734.


21. Wiesner L, Kothe R, Ruther W. Anatomic evaluation of two different techniques for the percutaneous insertion of pedicle screws in the lumbar spine. Spine (Phila Pa 1976) 1999 24:1599ŌĆō1603. PMID: 10457581.


22. Wiesner L, Kothe R, Schulitz KP, Ruther W. Clinical evaluation and computed tomography scan analysis of screw tracts after percutaneous insertion of pedicle screws in the lumbar spine. Spine (Phila Pa 1976) 2000 25:615ŌĆō621. PMID: 10749639.


23. Yukawa Y, Kato F, Ito K, et al. Placement and complications of cervical pedicle screws in 144 cervical trauma patients using pedicle axis view techniques by fluoroscope. Eur Spine J 2009 18:1293ŌĆō1299. PMID: 19488794.



24. Yoshimoto H, Sato S, Hyakumachi T, Yanagibashi Y, Kanno T, Masuda T. Clinical accuracy of cervical pedicle screw insertion using lateral fluoroscopy: a radiographic analysis of the learning curve. Eur Spine J 2009 18:1326ŌĆō1334. PMID: 19653013.



25. Franke J, Greiner-Perth R, Boehm H, et al. Comparison of a minimally invasive procedure versus standard microscopic discotomy: a prospective randomised controlled clinical trial. Eur Spine J 2009 18:992ŌĆō1000. PMID: 19360440.



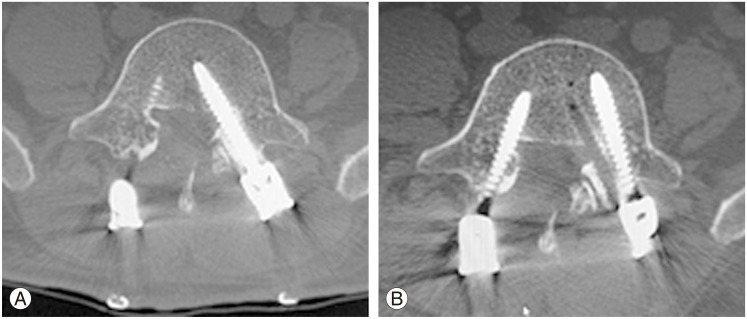
Fig.┬Ā1
Obliquity of fluoroscopy was chosen on the basis of preoperative computed tomography (CT) (group M-2). (A) Insertion angle (╬▒) and screw length (╬▓) were measured by subtracting the angle between the line passing through the centre of the pedicle before surgery, using axial CTs. (B) Obliquity of fluoroscopy was adjusted to be equal to the measured insertion angle (╬▒). (C) Radiographs obtained in the patients who underwent L3ŌĆō4 minimally invasive surgery-transpedicular lumbar interbody fusion. The true pedicle axis and the cephalad facet complex can be clearly seen, and the accurate insertion of pedicle screws was possible.
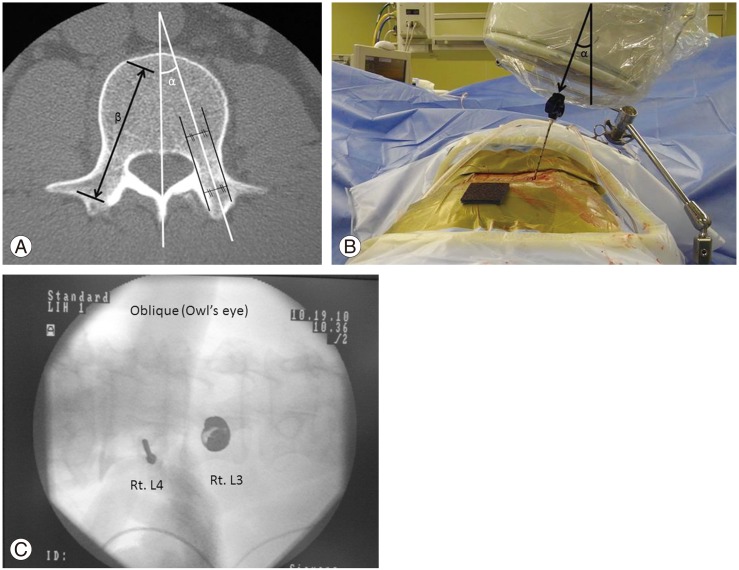
Fig.┬Ā2
The relative positions of the screws to the pedicles were assessed and classified using axial and reconstructed sagittal or coronal computed tomography as: A, completely within the pedicle; B, pedicle wall breach <2 mm; C, pedicle wall breach of 2ŌĆō4 mm; or D, pedicle wall breach >4 mm.
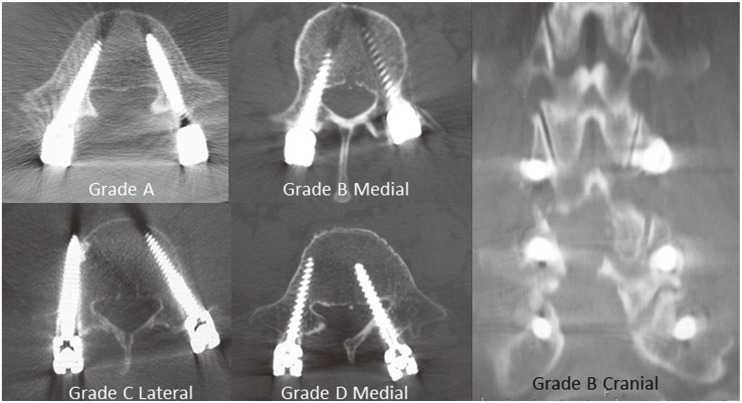
Fig.┬Ā3
(A) Computed tomography obtained for a 58-year-old male patient who underwent L4ŌĆō5 minimally invasive surgery-transpedicular lumbar interbody fusion using anterior-posterior and lateral fluoroscopic views (group M-1). Postoperatively medial grade D malposition of left L5 pedicle screw was revealed from his left L5 radiculopathy. (B) This screw was re-inserted in an additional surgery.