Risk of New Vertebral Fracture and Combination Therapy with Zoledronic Acid and Teriparatide in Diabetic Patients after Percutaneous Kyphoplasty
Article information
Abstract
Study Design
This was a retrospective clinical study.
Purpose
This study aimed to evaluate the effect of combination therapy with zoledronic acid and teriparatide on the risk of new vertebral fracture (NVF) in type 2 diabetes mellitus (T2DM) patients after percutaneous kyphoplasty (PKP).
Overview of Literature
Although T2DM had been associated with bone fragility and increased fracture risk, it remains unknown whether patients with T2DM could expect similar benefit from the combination therapy with zoledronic acid and teriparatide following PKP.
Methods
Total 106 diabetic patients who had undergone PKP and had received anti-osteoporosis treatment for osteoporotic vertebral compression fracture were enrolled and allocated into the following two groups: group I (n=52, zoledronic acid) and group II (n=54, zoledronic acid plus teriparatide). The operating time, bone cement volume, and complications related to anti-osteoporosis treatment or PKP, if any, were recorded. The Visual Analog Scale (VAS) score and Oswestry Disability Index (ODI) were assessed at admission, at discharge, and at the final follow-up. Dual-energy X-ray absorptiometry scan of the hip for the measurement of the bone mineral density (BMD) was performed preoperatively and at the final follow-up for all the patients.
Results
There was no significant difference in the age, body mass index, bone cement volume, or follow-up time of the groups. The mean follow-up duration was 22.5±1.6 months. All the patients had improved VAS and ODI, and group II had significantly better clinical outcomes than group I. All the patients had increased BMD at the latest follow-up, while group II exhibited significantly more improvement. The prevalence of NVF was lower in group II (11.5% vs. 7.4%, p=0.523). Male patients had a higher prevalence of NVF although the difference was not statistically significant.
Conclusions
Combination therapy with zoledronic acid and teriparatide could improve the clinical outcomes, and BMD and had the potential to reduce NVF in diabetic patients following PKP.
Introduction
China has the largest population of diabetes in the world and ranks first in terms of the prevalence of type 2 diabetes mellitus (T2DM), about 11% [1,2]. Research has shown that T2DM patients are a higher risk of osteoporosis vertebral compression fracture (OVCF) [3].
Percutaneous kyphoplasty (PKP) is a classic surgical treatment for OVCF and can alleviate pain and stabilize the vertebra rapidly. New vertebral fracture (NVF) after PKP was not uncommon and the most important steps for reducing the prevalence of NVF are treating osteoporosis and improving bone mineral density (BMD) [4,5]. In particular, patients with diabetes have an increased mortality rate and effective anti-osteoporosis therapy is required for diabetic patients after PKP [3].
The anti-osteoporotic medication could be divided in two categories. One includes the use of antiresorptive agents, such as bisphosphonates and denosumab, that inhibit both, bone resorption and formation. The other involves the use of anabolic agents, such as parathyroid hormone (PTH) and its analogs, that promote both, bone resorption and formation. Unlike other chronic diseases, such as hypertension and diabetes, combination therapy with different anti-osteoporosis drugs remains controversial [6]. Previous studies have indicated that the concurrent use of bisphosphonate might lower the anabolic effect of teriparatide [7,8]. However, subsequent studies have shown that the inhibitory effect might differ substantially when bisphosphonates were administered less frequently [9]. Zoledronic acid is a bisphosphonate that is administered annually, and teriparatide is the 1–34 fragment of PTH used daily, both of which are proven effective and safe for increasing BMD and reducing the fracture risk [10]. Cosman et al. [9] conducted a randomized controlled trial to compare the effect of zoledronic acid plus teriparatide, teriparatide alone, and zoledronic alone in postmenopausal osteoporosis and found that increases in spine BMD were 7.5%, 7.0%, and 4.5%, respectively, while increases in hip BMD were 2.3%, 1.1%, and 2.2%, respectively. Thus, the author held an affirmative attitude toward combination therapy with zoledronic acid and teriparatide [9].
However, because of limited evidence, combination therapy with zoledronic acid and teriparatide remained to be verified and have not been reported in diabetic patients after PKP. The present study was designed with the objective of determining whether combination therapy with zoledronic acid and teriparatide would improve the clinical outcomes and BMD and reduce NVF in diabetic patients following PKP.
Materials and Methods
This study was performed by conducting a retrospective analysis of the clinical and radiologic data. Informed consent was obtained from all individual participants included in the study at admission and approval was obtained from the institutional review board (IRB) of Shenzhen Second People’s Hospital (IRB approval no., 20190605009).
1. Study population and treatment protocol
From January 2017 to December 2017, diabetic patients who had received PKP and zoledronic acid alone or a combination of zoledronic acid and teriparatide because of acute OVCF were enrolled. The following excluding criteria were applied: history of anti-osteoporosis treatment; previous history of osteoporotic fracture; previous spinal surgery; diagnosis of other pathologic fractures, such as those related to malignancies; infections; or hepatorenal insufficiency. Total 106 patients were enrolled and allocated into the following two groups: group I (n=52, zoledronic acid), group II (n=54, zoledronic acid combined with teriparatide). All the patients took daily calcium 1,000 mg and 800 IU vitamin D. Patients were allowed ambulation with a soft brace 6 hours after PKP. On the first day after PKP, all the patients received infusion of 5 mg zoledronic acid dissolved in 100 mL saline and would receive another infusion after 12 months. The patients received infusion of 750 mL saline and took 0.3 g ibuprofen orally before the administration of zoledronic acid. Three months after the infusion of zoledronic acid, the patients in group II received 20 ug teriparatide subcutaneously daily. Baseline data on age, sex, body mass index (BMI), fracture level, operating time, bone cement volume, and complications related to OVCF or PKP, if any, were recorded.
2. Assessments
The Visual Analog Scale (VAS) and Oswestry Disability Index (ODI) were applied at the time of admission, at discharge, and at the final follow-up. All the patients underwent dual-energy X-ray absorptiometry scan of the lumbar spine and hip at admission; however, they underwent a scan of the hip alone at the final follow-up for the measurement of BMD. If a patient had back pain and suspected OVCF, a magnetic resonance scan was prescribed for verification. Complications related to anti-osteoporosis medication were also recorded.
3. Statistical analyses
Data are presented as mean±standard deviation values. Continuous data, such as those regarding age, follow-up time, BMI, operation time, bone cement volume, VAS score, ODI, and BMD T score were analyzed using t-test. Categorical variables, such as sex and NVF, were analyzed using chi-square test. Statistical analyses were conducted using IBM SPSS software ver. 24.0 (IBM Corp., Armonk, NY, USA). Statistical significance was set at p<0.05.
Results
1. Demographic characteristics
There was no significant difference in the average age (65.7±8.1 versus 66.8±8.2 years), BMI (23.3±3.2 versus 24.2±3.6 kg/m2), bone cement volume (4.1±0.4 versus 4.2±0.8 mL), follow-up time, operation time, or distribution of fracture location between the groups (Table 1). There was no significant difference in the hemoglobin A1c value of NVF and non-NVF in group I (7.4±2.2 versus 7.2±3.1, p=0.958). Patients with diabetic complications in the kidney, retina, and nerve were not included.
2. Clinical outcomes
The admission VAS score and ODI of the groups were similar. They were significantly lower in group II at the last follow-up (VAS score: 1.9±0.8 versus 1.2±0.4, p<0.001; ODI: 15.8%±3.7% versus 11.9%±4.8%, p<0.001), and the improvements were −4.1±1.5 versus −5.2±1.2 (p<0.001) and 40.1%±4.3% versus 45.6%±3.2% (p<0.001), respectively.
Both, female and male patients in group II had significantly better VAS scores (Fig. 1A, B) and ODI (Fig. 2A, B) at the final follow-up, while there was no significant difference between the female and male patients in group I or group II (Fig. 1C, D and Fig. 2C, D).
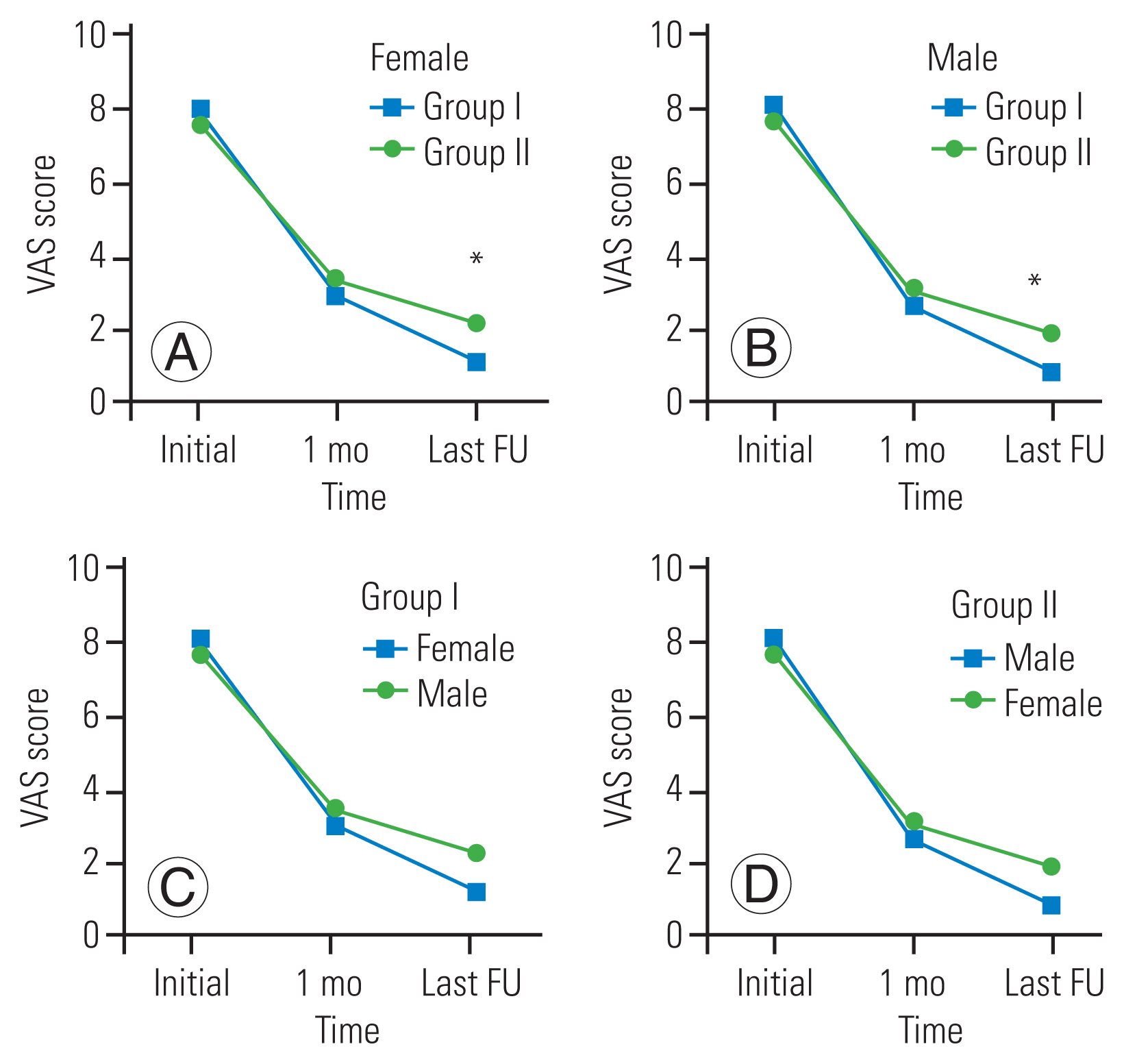
Clinical outcomes of Visual Analog Scale (VAS) score. (A) Comparison of VAS score of female patients between groups at different time points. (B) Comparison of VAS score of male patients between groups at different time points. (C) Comparison of VAS score between female and male patients in group I at different time points. (D) Comparison of VAS score between female and male patients in group II at different time points. FU, follow-up. *p<0.05.

Clinical outcomes of Oswestry Disability Index (ODI). (A) Comparison of ODI of female patients between groups at different time points. (B) Comparison of ODI of male patients between groups at different time points. (C) Comparison of ODI between female and male patients in group I at different time points. (D) Comparison of ODI between female and male patients in group II at different time points. FU, follow-up. *p<0.05.
Patients in the group I and II had similar baseline hip BMD (−3.1±0.3 versus −3.2±0.3, respectively; p=0.231) at admission (Table 1), while those in group II had higher BMD than those in group I at the final follow-up (−2.5±0.5 versus −2.2±0.4, p<0.001), with improvements of 0.5±0.1 and 0.7±0.2, respectively (p<0.000).
The hip BMD T score and BMD improvement in both, female and male patients was better in group II (Fig. 3A, B); however, there was no significant difference between the female and male patients in group I or group II (Fig. 3C, D).
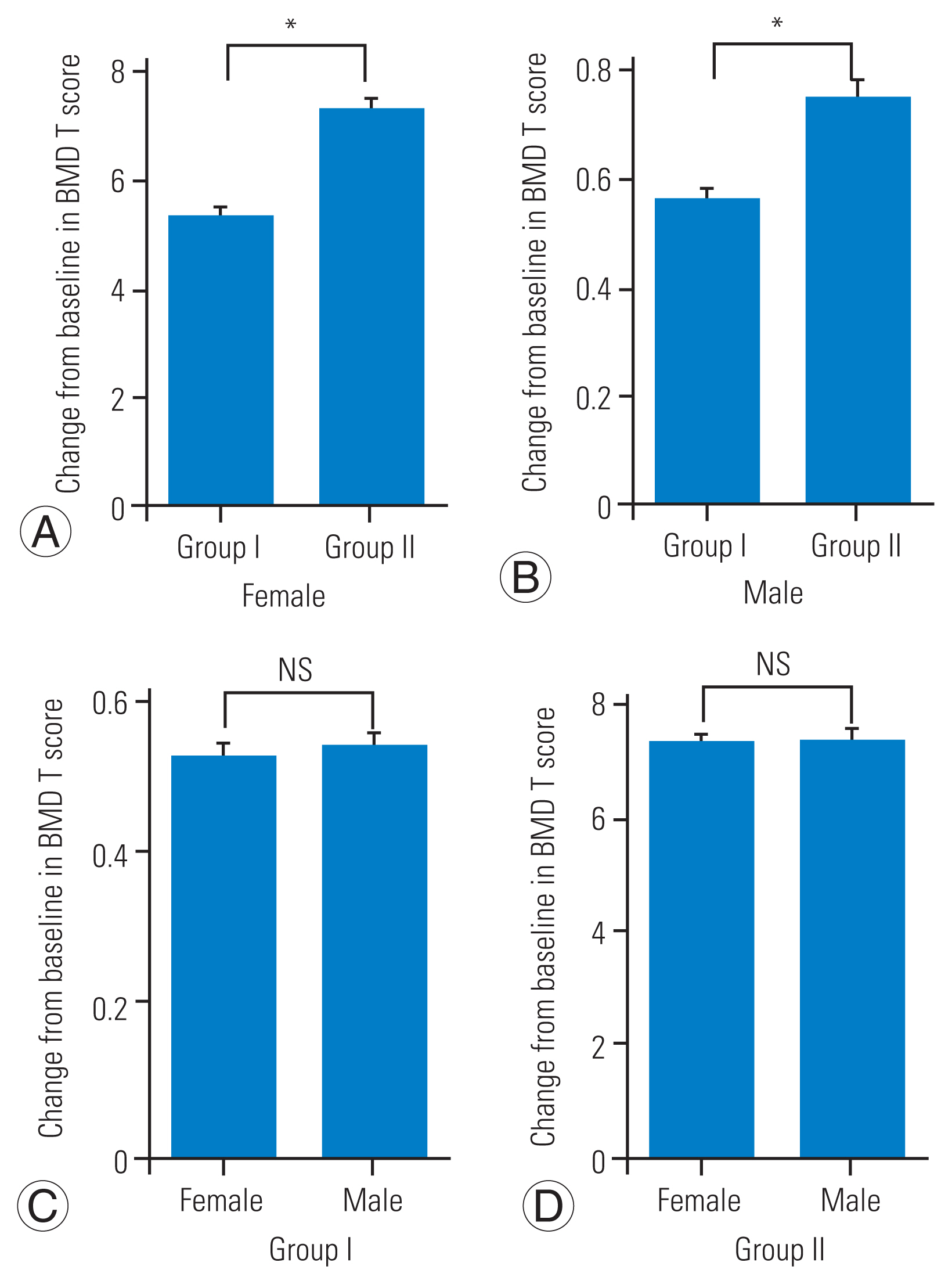
Improvement of bone mineral density (BMD). (A) Comparison of BMD of female patients between groups at admission and final follow-up (FU). (B) Comparison of BMD of male patients between groups at admission and final FU. (C) Comparison of BMD between female and male patients in group I at admission and final FU. (D) Comparison of BMD between female and male patients in group II at admission and final FU. NS, not significant. *p<0.05.
3. New vertebral fracture
Six patients in group I (two adjacent and four nonadjacent NVF) and four in group II (two adjacent and two nonadjacent NVF) had NVF. The NVF prevalence was lower in group II; however, the difference was not statistically significant (11.5% versus 7.4%, p=0.523). Both, female and male patients in group II had a lower prevalence, while male patients had a higher prevalence of NVF than female patients in both the groups (14.3% versus 10.5% in group I and 11.1% versus 5.6% in group II), although the differences were not significant (Fig. 4A–D). The duration between the NVF and PKP was 8.4±3.2 months in group I and 9.2±2.1 months in group II (p=0.130).
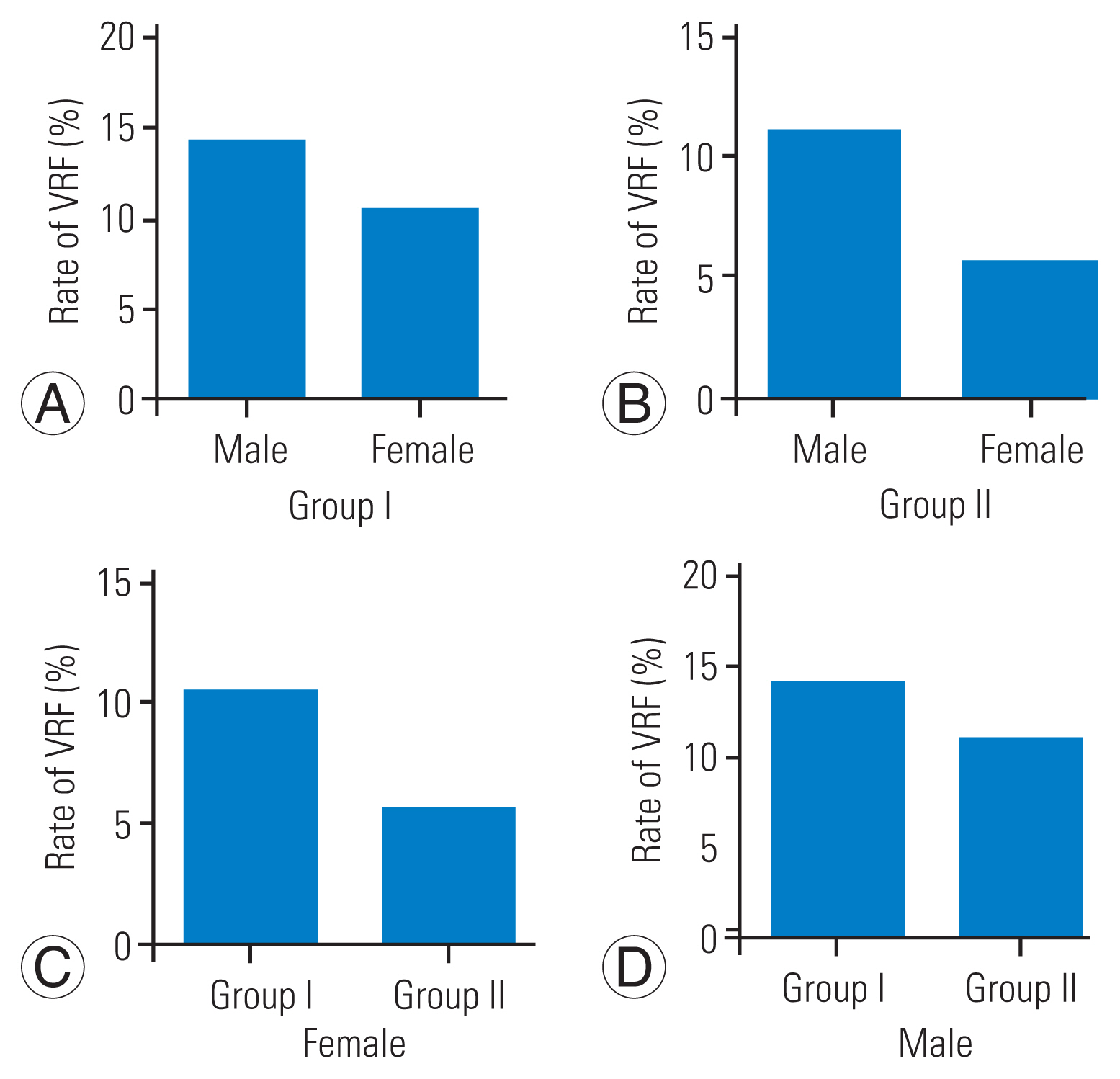
Prevalence of new vertebral fracture. (A) In the group I, the rate of vertebral refracture (VRF) was significant lower for female than male. (B) In the group II, the rate of VRF was significant lower for female than male. (C) The rate of VRF for female in group I is higher than group II. (D) The rate of VRF for male in group I is higher than group II.
Discussion
Partially attributed to the stiff cement, NVF was a common complication of PKP [11]. The reported prevalence of NVF following PKP was 20.8% (31/149) in the study by Boonen et al. [12] during the 2-year follow-up. Liu et al. [13] also reported eight cases of adjacent vertebral fracture and four cases of nonadjacent vertebral fracture in 50 patients who were treated with PKP; almost all the new fractures occurred within 1 year of PKP. Anti-osteoporosis treatment would reduce the NVF risk. Zoledronic acid is an antiresorptive agent that plays an important role in the prevention of vertebral fractures because it has a short time-to-onset for reducing vertebral fractures and high patient compliance [14]. In the present study, for diabetes patients who have undergone PKP and were proven to be at high risk of NVF in several studies, the prevalence of NVF was 11.1% when zoledronic acid was administered, much lower than that reported previously.
T2DM is associated with a higher risk of fracture for various reasons, such as lower cortical BMD, impaired physical function, nocturia, and decreased vision due to retinopathy or cataract. The medications for T2DM treatment may also affect bone health [15–19]. Zhang et al. [20] performed a 1-year prospective study to investigate the clinical effects of zoledronic acid in combination with PKP for treating OVCF and found that there was no NVF in the patients receiving 5 mg zoledronic acid with 0.25 μg/day calcitriol and 600 mg/day calcium carbonate. However, 11.1% of the diabetic patients who had undergone PKP had NVF despite treatment with zoledronic acid, indicating that diabetic patients had a much higher risk of vertebral fracture. Thus, much more effective anti-osteoporosis treatment should be prescribed for T2DM patients who have undergone PKP because this patient population is at high risk of NVF.
Currently, there is no consensus for this special population; however, it appears reasonable to speculate that an ideal anti-osteoporosis treatment should increase new bone formation and inhibit bone resorption. As we have mentioned above, although combination therapy of osteoporosis remains controversial, it still interested many researchers who were dedicated to exploring more effective treatment for patients with high risk of OVCF. The present study aimed to explore the combination therapy of zoledronic acid with teriparatide in a particular population of T2DM patients who had undergone PKP. Considering that the inhibiting effect of zoledronic acid (indicated by serum beta-C-terminal telopeptide) would peak in the 4th week [9], teriparatide was administered 3 months after zoledronic acid. We found that T2DM patients who had undergone PKP and were treated with a combination therapy had better BMD than those treated with zoledronic acid alone. Furthermore, patients treated with combination therapy had lower prevalence of NVF, although the difference was not significant. This current study confirmed the advantages of the combination therapy.
Total 27%–30% of all OVCF patients were men [21], and the mortality rate after osteoporotic fractures in men was much higher than that in women [22,23]. However, anti-osteoporosis treatment for men remains controversial owing to weak evidence [21]. Both, zoledronic acid and teriparatide reportedly increase the BMD significantly in men [24,25]; however, these drugs may not lower the risk of vertebral fracture. Boonen et al. [26] performed a multicenter, double-blind, placebo-controlled trial and randomly assigned 1,199 men with osteoporosis to receive infusion of 5 mg zoledronic acid or placebo at baseline and at 12 months; the authors observed an 81% risk reduction in moderate-to-severe vertebral fractures. However, the difference was not significant when morphologic or mild NVF was included. For teriparatide, Kaufman et al. [27] also found that teriparatide significantly reduced the risk of moderate or severe vertebral fracture by 83%; however, there was no significant reduction in the risk of all vertebral fractures. Some other authors have reported similar outcomes [21]. In the present study, male patients who were treated with zoledronic acid as well as those who were administered combination therapy had an obviously higher risk of NVF; however, this difference was not significant. Thus, zoledronic acid and teriparatide were less effective in men, and more effective anti-osteoporosis medications are required for male patients, especially those who have undergone PKP and have T2DM.
The definite advantage of the combination therapy demonstrated in this study was better pain relief. Min et al. [28] also reported that patients receiving teriparatide after OVCF showed more improvement in the numerical rating scale score than those who were administered bisphosphonate after 3 months. The palliative effect of teriparatide has also been reported by a study of Tsuchie et al. [29]. This effect might be because teriparatide has the ability to promote bone healing and pain relief [30].
Zoledronic acid and teriparatide are safe and well tolerated [31]. The adverse events in the present study included fever, myalgia, headache, injection-site tenderness, and nausea. No new or serious adverse events were observed in the combination therapy.
The retrospective study design, relatively small sample size, and lack of monitoring of the biochemical marker of bone turnover are the limitations of this study.
Conclusions
Combination therapy with zoledronic acid and teriparatide could improve the clinical outcomes and has the potential to reduce the prevalence of NVF in diabetic patients who have undergone PKP.
Notes
Conflict of Interest
No potential conflict of interest relevant to this article was reported.
