 |
 |
- Search
| Asian Spine J > Volume 15(6); 2021 > Article |
|
Abstract
Purpose
To compare the functional and radiological outcomes of anterior cervical discectomy and fusion (ACDF) using local graft and allograft
Overview of Literature
The choice of bone grafts for ACDF varies among different types: iliac crest, allograft, and substitutes. Availability, cost, and donor site morbidity are potential disadvantages. Local osteophyte grafts are then advantageous and shows to have good fusion.
Methods
We randomly sampled participants requiring a single level ACDF for degenerative conditions (n=27) between allograft (n=13) and local graft (n=14) groups. Follow-up of patients occurred at 6 weeks, 3 months, 6 months, and 1 year using Numerical Pain Rating Scale (NPRS) scores for arm and neck pain, Neck Disability Index (NDI), 2-item Short Form Health Survey (SF-12), and lateral disk height. We then assessed radiological fusion using computed tomography (CT) scan at 12 months, and graded as FŌłÆ (no fusion), F (fusion seen through the cage), F+ (fusion seen through the cage, with bridging bone at one lateral edge), and F++ (fusion seen through cage with bridging bone bilaterally).
Results
There were no significant differences in the age, sex, duration of intervention, blood loss, and hospital stay between the two groups (p>0.05). Both groups showed significant improvements in all functional outcome scores including NPRS for arm and neck pain, NDI, and SF-12 at each visit (p<0.01). We observed a marked improvement in disk height in both groups (p<0.05), but at 1 year of follow-up, there was a significant though slight subsidence (p=0.47). CT at 1 year showed no non-unions. We recorded F, F+, and F++ grades of fusion in 23.2%, 38.4%, and 38.4% in allograft group and 28.6%, 42.8%, and 28.6% in local graft group, respectively, though no significant differences observed (p=0.73).
Anterior cervical discectomy and fusion (ACDF) is a highly effective surgical procedure used to manage radiculopathy in order to regain functional activities. Removing the herniated disc fragment entails removal of the rest of the nucleus pulposus and the anterior annulus. After discectomy and nerve root decompression, the management of the vacant disk space has been controversial for many years. Ranging from leaving the disk space free [1], to filling the disc space with bone grafts [2ŌĆō4] and cage [5,6], and the addition of a cervical plate [7,8], many treatment options have been described with similar outcomes.
Use of a cage as a stand-alone fixation is a popular choice among surgeons for ACDF [5,9ŌĆō11] and several studies reveal good outcomes with the use of stand-alone titanium cages [11,12]. The use of synthetic cages in disc space compared to the autograft alone is in their ability to succumb better load transmission between adjacent vertebral bodies, facilitate insertion, and maintain disc height and structural support [9,10]. However, the choice of bone grafts used was diverse, including iliac crest autograft, allograft, and graft substitutes. Iliac crest autograft is an excellent option considering its osteogenic and osteoconductive properties. But donor site morbidity, the need for an additional incision and increased surgical duration are potential disadvantages to its practice compared to other forms [13]. Allografts on the other hand, have these corresponding advantages [4]. However, its availability is not universal in many surgical centers.
Local osteophytes and the antero-inferior lip of proximal vertebra are often nibbled during ACDF, which can be used as graft fillers inside the cage. Such local osteophyte grafts lack the disadvantages of iliac crest autograft and allograft. Few studies on local graft (LG) have shown to have good fusion characteristics as well [14ŌĆō16]. However, there are no randomized controlled trials to compare the adequacy, efficacy, and outcomes of local osteophyte grafts, to the best of our knowledge. We performed a randomized controlled trial to compare clinical, functional and radiological outcomes of ACDF using LG group and allograft group.
The Institutional Review Board of Ganga Medical Centre and Hospitals, Coimbatore, India approved our study with reference number 26012018/GMCH/IRB. We randomly sampled patients (n=32) requiring single level ACDF for non-traumatic conditions between August 2017 and September 2018, between allograft and LG after signing an informed detailed consent. The patient selection, allocation, intervention, follow-up, and assessment were performed as per CONSORT (Consolidated Standards of Reporting Trials) guidelines (Fig. 1). The randomization numbers were generated by a computer-generated random chart. We excluded participants having more than two levels of disease, adjacent segment disease with previous surgical intervention, patients with history, and clinical features of trauma, tumor, infection, inflammation, and those with American Society of Anesthesiologists grading >3 from the study.
A single surgeon operated upon all the patients. The surgical procedure was standard in both groups with a right sided Smith Robinson approach. After discectomy, an appropriately sized titanium cage (stand alone, contoured for end plates with serrations, and a central axial hole for packing bone graft) was chosen. In LG group, the antero-inferior lip of the superior vertebra and osteophytes if present near the affected disk was nibbled with No. 3 bone punch rongeur. Then, we prepared bone pieces into small bone chunks to be packed into the titanium cage. In the allograft group, we packed free fragments of cancellous allograft (freeze dried from bone bank) mixed with patientŌĆÖs effusing blood into the cage. No anterior cervical plates were used in any of the patients. A hard-cervical collar was provided for 2 weeks. Follow-up occurred at 6 weeks, 3 months, 6 months, and 1 year following intervention. Preoperatively and at each visit, we documented pain scores for arm and neck pain, Neck Disability Index (NDI), and 2-item Short Form Health Survey (SF-12) by an independent observer. We also calculated the segmental disk height at the mid-disk level (midway between anterior and posterior ends of disk space in the lateral radiograph) (Fig. 2). In addition, we assessed radiological fusion by computed tomography (CT) scan at 12 months. Fusion was graded as FŌłÆ (no fusion), F (fusion seen through the cage in the coronal or sagittal image), F+ (fusion seen through the cage along with bridging bone at one lateral edge in the coronal image), and F++ (fusion seen through cage with bridging bone bilaterally in the coronal image) (Fig. 3). Two observers independently evaluated all follow-up CT images performed at 12 months (a musculo-skeletal radiology fellow and a fellowship trained spine surgeon). Any differences in the observation were settled by consensus between them before the final analysis. The mean kappa value for intra-observer reliability was 0.82 (excellent) and inter-observer reliability was 0.76 (substantial).
We performed sample size calculation based on the expected difference in mean Numerical Pain Rating Scale (NPRS) and disk height among the two study groups at 12 months postoperative period. We assumed one standard deviation (SD) difference in mean NPRS between allograft and LG groups, power of 80% and ╬▒ of 0.05. Based on this, the expected sample was 15 in each of the two groups meaning a total sample size was of 30. We also assumed one SD difference in the mean disc height between the two groups. With a sample size of 30 and ╬▒ of 0.05, we were able to achieve a power of 80%.
We performed data entry and analyses by IBM SPSS ver. 21.0 (IBM Corp., Armonk, NY, USA). We analyzed output indicators through the software and we described results in form of tables and graphs. We calculated the mean (SD) or median (interquartile range) for continuous variables and proportions for categorical variables. We compared proportions using chi-square test whereas we compared means using Mann-Whitney U-test. Then, we generated bar graphs and pie charts using excel sheets. For all comparisons, the p-values <0.05 were considered statistically significant.
There were 32 patients eligible for the study out of which 27 completed 1-year follow-up (three patients refused further participation and two were lost to follow-up). Twenty-one patients were diagnosed as radiculopathy and six were diagnosed as myelopathy. Among 27 patients, 13 were in the allograft group and 14 in the LG group.
The mean age of participants receiving allograft was 41.9┬▒7.1 years and for those receiving LG, it was 44.7┬▒10.4 years. The mean age was similar across the two groups (p=0.32). The distribution of participants by sex was similar across the two groups as well. In those receiving allografts, 76.9% were males and remaining 23.1% were females. In those receiving LG, 64.3% were males and 35.7% were females. There were no significant differences in the duration of surgery, blood loss, and hospital stay between the two groups (p>0.05) (Table 1).
Both groups showed significant improvements in all the functional scores including NPRS for arm and neck pain, NDI, SF-12 score at each visit (p<0.01), and this was maintained at one year of follow-up (Table 2). When comparing the improvement of NPRS score of arm and neck pain between the two groups, there were no significant differences till the 3-month follow-up period. However, at the 6-month and 12-month follow-up, patients in LG group were significantly better when compared to the allograft group. Similarly, the SF-12 scores and the NDI also showed similar trends with both groups compared to their preoperative values. Between the two groups, there were no significant differences until the 6-month follow-up period. At 12 months, the LG group fared significantly better although the mean values of allograft group were significantly better than the preoperative values.
There was a significant improvement in disk height from preoperative to postoperative period in both groups (Table 3). The mean preoperative disk height was 3.94 mm and 4.32 mm for allograft and LG, respectively, which improved to 6.67 mm and 6.86 mm at immediate postoperative period. There was a mild loss of disk height at the final follow-up (5.5 mm and 5.76 mm, respectively). There was no significant difference in disk height between allograft and LG group at preoperative and all postoperative visits.
At 1-year follow-up with CT, there were no non-unions. And 23.2% showed F grade, 38.4% F+ grade, and 38.4% F++ grade of fusion in the allograft group. Meanwhile 28.6% showed F grade, 42.8% showed F+ grade, and 28.6% F++ grades of fusion in the LG group (Fig. 4). There were no significant differences in the grade of fusion on CT scan at 12 months postoperatively between the two groups (p=0.73) (Table 3).
To the best of our knowledge, this is the first randomized controlled trial comparing the efficacy of local bone grafts with allografts in the treatment of cervical disk herniation. The study showed that both techniques provide significant improvements in arm and neck pain, which are primary goals of treatment in patients with disk herniation and radiculopathy. Secondly, there was radiological evidence of fusion in one or more zones of the intervertebral disc in all patients treated by either of the techniques. Thus, local osteophyte grafts can be considered as an alternate to allografts or even as a standard choice of graft material in patients undergoing single level ACDF.
After a discectomy, the defect in the intervertebral space is filled with one of the following: autograft, allograft, cage, or artificial disk [2,6,16ŌĆō18]. Hypertrophic marginal osteophytes around cervical vertebrae obtained at the time of surgery can be used as graft material to fill the cage. Local osteophyte graft reduces the additional cost associated with allograft and the morbidity associated with iliac crest graft. Studies show that removal of bone plugs around vertebrae does not change compressive strength or mechanical strength of cervical spine. Hence, local osteophyte graft are being used as an alternative to traditional iliac crest graft or allografts [15]. Shad et al. [19] studied the use of cage and local autologous bone graft for ACDF in 22 patients. During the surgical procedure after the end plates preparation, bone dust mixed with blood is packed into the cage and inserted into the disk space. The authors revealed a significant improvement in functional scores after surgery. Radiological evaluation showed significant changes in both local and regional kyphotic angles and increase in segmental height. Subsequently, Pitzen et al. [16] in 2006 conducted a prospective study on filling a cervical spine cage with local autograft in 21 patients. Results of their study revealed a significant increase in bone density and bone fusion was noted in 91.3% of cases [16].
Our study compares clinical, functional, and radiological outcomes of ACDF using cage with allograft and local osteophyte graft. Very few studies have compared the clinical and functional outcomes of LGs with allografts and iliac crest graft. Liu et al. [20] in 2017 conducted a study comparing local bone graft with PEEK (polyetheretherketone) cage versus iliac crest bone graft in ACDF. Among 60 consecutive patients divided into two groups, the authors showed similar improvements in Visual Analog Scale score for pain, disc height restoration, and fusion rate between the two groups.
In the current study, we performed a randomized control trial comparing LG and allografts, which is probably the first of its kind. Both groups demonstrated significant improvements in functional outcome scores (NPRS for neck, NPRS for arm, NDI, SF-12) after surgery. Although the pain scores at 12 months (mean NPRS=1.1) in the allograft group was very low and significantly better than the preoperative values (mean NPRS=6.9), there were significant differences when compared with the LG group. We observed that two patients in the allograft group had pre-existing disk degeneration at other cervical levels, which probably contributed to the slightly higher values in the allograft group. In hindsight, it appears valid that they should have been excluded. Fortunately, a large study population would have negated the influence of such outliers.
The fusion rates best reflect the long-term radiological outcomes after ACDF. We used CT imaging to analyze fusion at the end of 1 year. Fusion was graded as F, F+, and F++ in the coronal images. We did not rely on sagittal images alone, as the footprint of the cage used was similar in dimension to the endplate. Hence, fusion occurring anteriorly or posteriorly to the cage may not be appreciated. Both groups showed good fusion happening through the cage in all the patients. Among allograft group, 23.2% had F, 38.4% had F+, and 38.4% had F++. Among local osteophyte graft group, 28.6% had F, 42.8% had F+, and 28.6% had F++. The difference in proportions was not significant (p-value=0.73). Use of CT scan is a standard technique for assessing fusion status after spinal fusion surgery. In the context of anterior cervical fusion, the use of CT scan has been endorsed in previous studies and found to have higher specificity for evaluating fusion than radiographs and MRI [21]. We have also included the presence of both intra-cage and extra-cage bone bridging in our assessment method of ACDF [22]. To ascribe a gradation to the presence of bridging bone circumferentially around the cage and within the cage, we have graded the strength of fusion as FŌłÆ to F++.
The study has some limitations. Firstly, our sample size was not sufficient. We calculated the sample size to be 30 based on presumed one SD difference in NPRS and disk height between the two groups. The strength of the study mainly lies in its randomized design with blinded observers. Secondly, the study had only two arms: allograft and local osteophytes. Additional arms such as iliac crest graft or discectomy alone, would improve strength to the study. A large multi-center trial involving a large sample size with multiple arms would be beneficial and are recommended to add strength to the observations.
Marginal osteophytes obtained during of surgery, can be used as graft material for ACDF, since they provide similar radiological outcomes, and improvements in clinical and functional outcomes compared to allografts. The local osteophyte grafts are cost effective since they are obtained during surgery and avoid problems of donor site complications, additional costs, and risks of disease transmission. Concerns regarding their efficacy in achieving fusion have been addressed in this study.
Conflict of Interest
Conflict of Interest
No potential conflict of interest relevant to this article was reported.
Notes
Author Contributions
All authors contributed equally towards the preparation of this manuscript.
Notes
Funding
We received funding from the Ganga Orthopedic Research and Education Foundation (GOREF).
Fig.┬Ā1
The patientsŌĆÖ selection, allocation, intervention, follow-up, and assessment were performed as per CONSORT guidelines. CONSORT, Consolidated Standards of Reporting Trials.

Fig.┬Ā2
Lateral radiograph of the cervical spine before (A) and after surgery (B). The segmental disc height is calculated at the mid-disc level, midway between anterior and posterior ends of disc space.
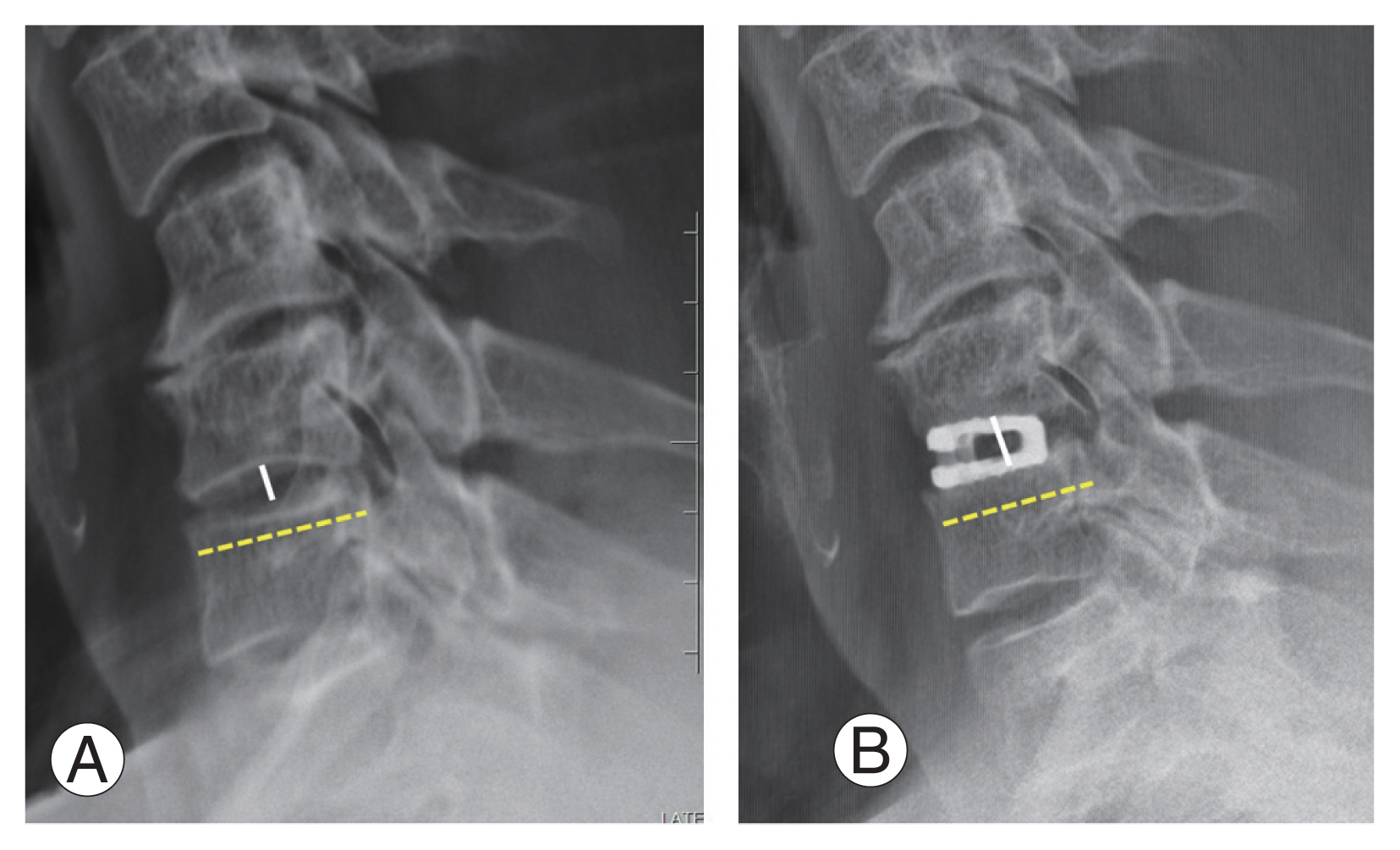
Fig.┬Ā3
Coronal computed tomography images were evaluated for the evidence of fusion at the end of 1 year. (A) F: fusion seen through the cage in the coronal or sagittal image. (B) F+: fusion seen through the cage along with bridging bone at one lateral edge in the coronal image. (C) F++: fusion seen through cage with bridging bone bilaterally in the coronal image.
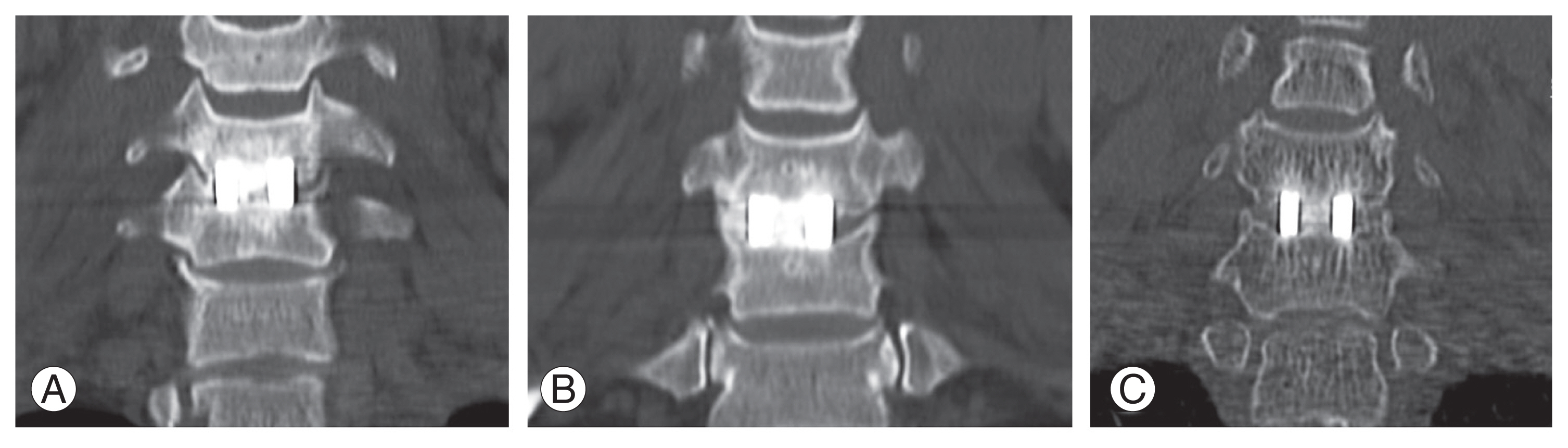
Fig.┬Ā4
This 45-year-old male presented with right C7 myeloradiculopathy due to C6ŌĆō7 disc osteophyte complex: (A) sagittal and (B) axial magnetic resonance images (arrow). (C) The lateral X-ray shows a congenital C2ŌĆō3 fusion. (D) He underwent C6ŌĆō7 anterior cervical discectomy and fusion with a stand-alone cage filled with local graft. Follow-up radiographs at 6 weeks (E), 3 months (F), and 1 year (G) show mild cage subsidence. (H) Computed tomography performed at 12 months shows fusion through the cage and right lateral zone (F+). (I) Sagittal image shows fusion occurring anterior and posterior to the cage as well.

Table┬Ā1
Demographics and surgical parameters
Table┬Ā2
Comparison of functional outcome scores between the two groups
Table┬Ā3
Comparison of radiological outcome scores between the two groups
References
1. Maurice-Williams RS, Dorward NL. Extended anterior cervical discectomy without fusion: a simple and sufficient operation for most cases of cervical degenerative disease. Br J Neurosurg 1996;10:261ŌĆō6.


2. Miller LE, Block JE. Safety and effectiveness of bone allografts in anterior cervical discectomy and fusion surgery. Spine (Phila Pa 1976) 2011;36:2045ŌĆō50.


3. Yue WM, Brodner W, Highland TR. Long-term results after anterior cervical discectomy and fusion with allograft and plating: a 5- to 11-year radiologic and clinical follow-up study. Spine (Phila Pa 1976) 2005;30:2138ŌĆō44.


4. An HS, Simpson JM, Glover JM, Stephany J. Comparison between allograft plus demineralized bone matrix versus autograft in anterior cervical fusion.: a prospective multicenter study. Spine (Phila Pa 1976) 1995;20:2211ŌĆō6.


5. Zhu D, Zhang D, Liu B, Li C, Zhu J. Can self-locking cages offer the same clinical outcomes as anterior cage-with-plate fixation for 3-level anterior cervical discectomy and fusion (ACDF) in mid-term follow-up? Med Sci Monit 2019;25:547ŌĆō57.



6. Park JI, Cho DC, Kim KT, Sung JK. Anterior cervical discectomy and fusion using a stand-alone polyetheretherketone cage packed with local autobone: assessment of bone fusion and subsidence. J Korean Neurosurg Soc 2013;54:189ŌĆō93.




7. Doria C, Mosele GR, Balsano M, Maestretti G, Caggiari G. Anterior decompression and plate fixation in treatment of cervical myelopathy: a multicentric retrospective review. Acta Orthop Traumatol Turc 2018;52:185ŌĆō90.



8. Zhang Z, Li Y, Jiang W. A comparison of zero-profile anchored spacer (ROI-C) and plate fixation in 2-level noncontiguous anterior cervical discectomy and fusion: a retrospective study. BMC Musculoskelet Disord 2018;19:119.




9. Hosoi K, Tonomura H, Takatori R, et al. Usefulness of anterior cervical fusion using titanium interbody cage for treatment of cervical degenerative disease with preoperative segmental kyphosis. Medicine (Baltimore) 2017;96:e774.

10. Moreland DB, Asch HL, Clabeaux DE, et al. Anterior cervical discectomy and fusion with implantable titanium cage: initial impressions, patient outcomes and comparison to fusion with allograft. Spine J 2004;4:184ŌĆō91.


11. Rohe SM, Engelhardt M, Harders A, Schmieder K. Anterior cervical discectomy and titanium cage fusion: 7-year follow-up. Cent Eur Neurosurg 2009;70:180ŌĆō6.



12. Li ZJ, Wang Y, Xu GJ, Tian P. Is PEEK cage better than titanium cage in anterior cervical discectomy and fusion surgery?: a meta-analysis. BMC Musculoskelet Disord 2016;17:379.



13. Arrington ED, Smith WJ, Chambers HG, Bucknell AL, Davino NA. Complications of iliac crest bone graft harvesting. Clin Orthop Relat Res 1996;(329): 300ŌĆō9.

14. Ekanayake J, Shad A. Use of the novel ANSPACH bone collector for bone autograft in anterior cervical discectomy and cage fusion. Acta Neurochir (Wien) 2010;152:651ŌĆō3.



15. Pitzen T, Tan JS, Dvorak MF, Fisher C, Oxland T. Local autograft retrieval from a cervical vertebral body: biomechanical consequences. J Neurosurg Spine 2012;16:340ŌĆō4.


16. Pitzen T, Kiefer R, Munchen D, Barbier D, Reith W, Steudel WI. Filling a cervical spine cage with local autograft: change of bone density and assessment of bony fusion. Zentralbl Neurochir 2006;67:8ŌĆō13.



17. Boselie TF, Willems PC, van Mameren H, de Bie R, Benzel EC, van Santbrink H. Arthroplasty versus fusion in single-level cervical degenerative disc disease. Cochrane Database Syst Rev 2012;(9): CD009173.


18. Park HW, Lee JK, Moon SJ, Seo SK, Lee JH, Kim SH. The efficacy of the synthetic interbody cage and Grafton for anterior cervical fusion. Spine (Phila Pa 1976) 2009;34:E591ŌĆō5.


19. Shad A, Leach JC, Teddy PJ, Cadoux-Hudson TA. Use of the Solis cage and local autologous bone graft for anterior cervical discectomy and fusion: early technical experience. J Neurosurg Spine 2005;2:116ŌĆō22.


20. Liu JM, Xiong X, Peng AF, et al. A comparison of local bone graft with PEEK cage versus iliac bone graft used in anterior cervical discectomy and fusion. Clin Neurol Neurosurg 2017;155:30ŌĆō5.








