Computed Tomographic Morphometric Analysis of C1 and C2 for Lamina Cross Screw Placement in Malay Ethnicity
Article information
Abstract
Study Design
This is an observational study of computed tomography (CT) data.
Purpose
The C1 and C2 laminas in the Malaysian Malay population were analyzed for the feasibility of fitting 3.5-mm laminar screws in a cross configuration.
Overview of Literature
Morphometric analysis of the C1 and C2 laminas has been performed for various populations but not for the Malaysian Malay population.
Methods
A total of 330 CT cervical images were measured to establish the bicortical diameter of the C1 and C2 laminas as well as their height and length. The C1 posterior tubercle bicortical diameter and height were also determined from these images. All parameters were measured up to 0.1 mm, and statistical analysis was performed using IBM SPSS Statistics ver. 24.0 (IBM Corp., Armonk, NY, USA). An independent t -test and the Pearson chi-square test were used to determine the mean difference and screw acceptance.
Results
The means of the C1 lamina measurements were 5.79±1.19 mm in diameter, 9.76±1.51 mm in height, and 20.70±1.86 mm in length. The means of the measurements of the posterior tubercle were 7.20±1.88 mm in diameter and 10.51±1.68 mm in height. The means of the C2 lamina measurements were 5.74±1.31 mm in diameter, 11.76±1.69 mm in height, and 24.96±2.56 mm in length. Overall 65.5% of C1 and 80.3% of C2 laminas are able to accept 3.5-mm screws in a cross configuration. Screw acceptability is similar between the right and left sides (p>0.05). However, males have a higher screw acceptability compared with females (p<0.05), except for the C2 left lamina.
Conclusions
It is feasible to insert a 3.5-mm screw in a cross configuration in the C1 and C2 laminas of the Malaysian Malay population, especially in males. However, a CT scan should be performed prior to the operation to determine screw acceptability and to estimate screw sizes.
Introduction
The atlantoaxial joint is a diarthrodial joint that contributes 50% of total neck rotation, and the atlanto-occipital joint contributes 50% of total neck flexion and extension. A number of conditions such as fractures, rheumatoid arthritis, tumors, infections, and ligamentous laxity can lead to instability of the atlantoaxial joint, which may lead to pain and neurological deficits. Cervical spine fractures comprise one third of all spine injuries, and C1/C2 fractures comprise one third of all cervical spine injuries. Although less than half of these injuries are treated surgically, they are more technically demanding.
Current treatment for atlantoaxial instability is stabilization via an anterior or posterior approach, in which the former is more technically demanding and has a high risk of retropharyngeal wound breakdown. Among the popular posterior stabilization methods are the C1–C2 transarticular screw, the C1 lateral mass screw with a C2 pedicle screw, the posterior wiring of C1–C2, C1–C2 interlaminar clamps, and occipitocervical fusion [1]. However the current techniques of stabilization either poses a risk to injuring the vertebral artery, are not stable enough, or cause loss of motion of the occipitocervical joint [2-5].
Current stabilization methods may not be feasible when there is vertebral artery anomaly, unilateral vertebral artery occlusion, or erosion of the lateral mass by a degenerative process or tumor invasion into the C1 lateral mass or C2 pedicle. This is due to the higher risk of injuring the vertebral artery or those risks associated when one of these factors involves the area where the screw is intended to be inserted [6-8].
C1–C2 laminar screw fixation has been introduced as a method of stabilization as it reduces the risk of injuring the vertebral artery and serves as an alternative procedure when another method of fixation is not possible [7-10]. However, there are limited studies on whether the Malaysian Malay population has a large enough lamina for the insertion of a 3.5-mm screw. This morphometric analysis is imperative, as our population may have a smaller morphometry compared with that of most studies performed with subjects from a western population [11-13].
Materials and Methods
Cervical computed tomography (CT) images of patients performed in the emergency department (new trauma cases) from 2015 to 2018 were retrieved from the picture archiving and communications system database. All Malaysian Malay patients of both genders aged 18–60 years were selected. Patients with the presence of C1 and/or C2 cervical vertebra fractures, infection, tumors, congenital abnormality, prior instrumentation, or artifacts in the images were excluded from the study. Out of the 372 cervical CT images, 42 were excluded from the study due to the presence of an unfused C1 posterior arch, fractures, or prior instrumentation.
Both C1 and C2 CT images were measured using the tool in the workstation Centricity Universal Viewer Web Client ver. 6.0 (GE Healthcare Malaysia, Kuala Lumpur, Malaysia) by one investigator to ensure consistency. The CT image slice was 1.0-mm thick and was reconstructed by correcting sagittal tilt, coronal tilt, and axial rotation to obtain a true axial and sagittal view for measurement.
Parameters measured from the axial view were the C1 and C2 laminas’ bicortical diameters and length and the C1 posterior tubercle bicortical diameter. The parameters measured from the sagittal view were the C1 and C2 lamina height and the C1 posterior tubercle height (Fig. 1). The C1 lamina was defined as the portion of the posterior arch that extends from the most posterior edge of the vertebral artery groove to the posterior tubercle, as defined by Kim et al. [14].
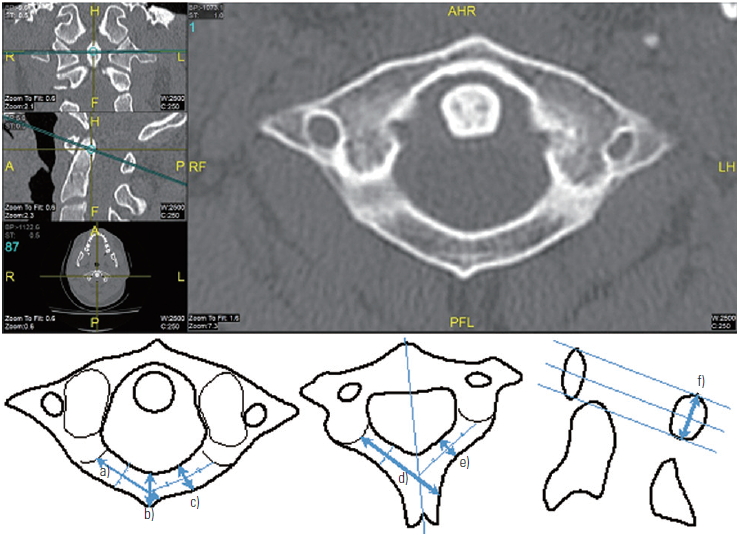
A computed tomography image showing a true axial view of Atlas after correction of tilt in the sagittal and coronal planes. The illustration shows how measurements are obtained for a)the C1 lamina length, b)C1 posterior tubercle bicortical diameter, c)C1 lamina bicortical dia meter, d)C2 lamina length, e)C2 lamina bicortical diameter, and f)the heights of the C1 and C2 laminas.
Assuming a 3.5-mm screw is being inserted with a margin of error of 0.5 mm on each side, it is deemed possible to insert a 3.5-mm screw if the lamina bicortical diameter is ≥4.5 mm, the height ≥4.5 mm, and the length ≥20 mm. It is feasible to insert screws in a cross configuration in C1 if the bilateral lamina and posterior tubercle bicortical diameters are ≥4.5 mm, the height is ≥9 mm, and the bilateral lamina length is ≥20 mm, whereas it is feasible to insert a screw in a cross configuration in C2 if the bilateral lamina bicortical diameter is ≥4.5 mm, the height is ≥9 mm, and the length is ≥20 mm.
Feasibility of screw insertion is presented as a percentage, and mean±standard deviation (SD) values are calculated for all parameters. Statistical analysis was performed with IBM SPSS Statistics ver. 24.0 (IBM Corp., Armonk, NY, USA). An independent t-test was used to determine the mean difference, and the Pearson chi-square test was used to test the difference between the screw acceptance rate by gender and between the right and left sides. A p-value of <0.05 was considered statistically significant.
This study has been approved by the Human Research Ethics Committee of Hospital Universiti Sains Malaysia (USM/JEPeM/18010007). Informed consent was obtained from all individual participants included in the study.
Results
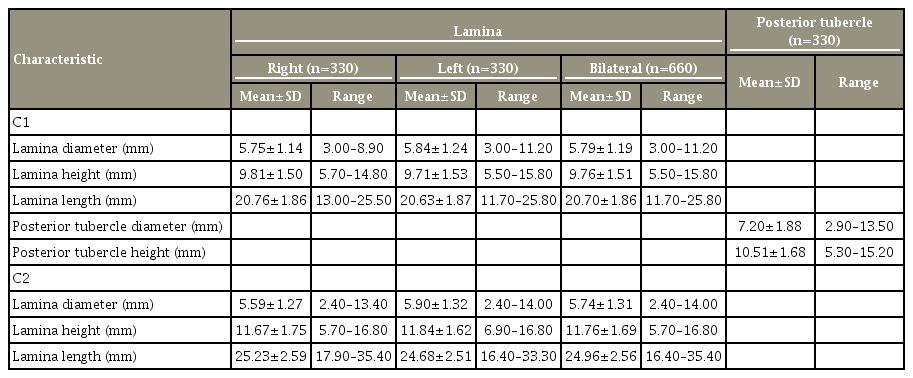
In total, 270 males (81.8%) and 60 females (18.2%) were included in our study. The patients’ ages ranged from 18 to 60 years, with a mean age of 34.13 years and median age of 32 years. The mean value and SD of the results of the measurement of height, bicortical diameter, and length of the C1 and C2 laminas, as well as the height and bicortical diameter of the C1 posterior tubercle, were summarized (Table 1).
The mean C1 lamina diameter was 5.75±1.14 mm for the right side and 5.84±1.24 mm for the left side, with 90.0% of the right side and 87.3% of the left side having a diameter of ≥4.5 mm. The mean diameter for the C2 lamina was 5.59±1.27 mm for the right side and 5.90±1.32 mm for the left side, with 85.8% of the right side and 89.4% of the left side having a diameter of ≥4.5 mm. The mean C1 posterior tubercle diameter was 7.20±1.88 mm, with 96.4% having a diameter of ≥4.5 mm.
The mean height of the C1 lamina was 9.81±1.50 mm and 9.71±1.53 mm for the right and left sides, respectively. C2, however, has a larger lamina height with a mean of 11.67±1.75 mm and 11.84±1.62 mm for the right and left sides, respectively. All C1 and C2 laminas must have a height of ≥4.5 mm to accept a laminar screw on both the right and left sides. For bilateral, cross screw placement, which requires a height of ≥9.0 mm, only 75.0% of the C1 lamina and 97.4% of the C2 lamina are able to accommodate the construct. The C1 posterior tubercle height has a higher bilateral cross screw acceptance rate compared with the C1 lamina, with 86.1% having a height of ≥9.0 mm and a mean of 10.51±1.68 mm.
The mean C1 lamina length was 20.76±1.86 mm on the right side and 20.63±1.87 mm on the left side, with 81.8% of the right side and 81.2% of the left side having a length of ≥20.0 mm. The C2 lamina has a mean length of 25.23±2.59 mm on the right side and 24.68±2.51 mm on the left side, with 99.7% and 99.4% having a length of ≥20.0 mm for the right and left sides, respectively.
In terms of the 3.5-mm screw acceptability according to the specified criteria, 79.4% of the C1 right lamina and 78.2% of the C1 left lamina were able to accommodate a 3.5-mm screw. However, only 65.5% of the C1 lamina were able to accept screws in a cross configuration. Screw acceptability of the C2 lamina was 85.8% and 88.8% for the right and left laminas, respectively, and acceptability for a screw in a cross configuration was 80.3%. Screw acceptability for 3.5-mm screws for both C1 and C2 was shown (Table 2).
Equal variances were tested using Levene’s test; if Levene’s significance p-value for equal variance was <0.05, then equal variances, not assumed values, were used. All parameters (diameter, height, and length) measured from C1 and C2 were found to be statistically significant, more so in the male population compared with that in the female population. The C1 posterior tubercle diameter showed similar results (p=0.066). The male population was also bound to have a higher screw acceptance rate compared with the female population, whether it was a unilateral lamina or a bilateral lamina, except for the C2 left lamina, which showed similar screw acceptability (p=0.139).
The C1 lamina diameter, height, and length measurements were found to be similar between the right and left sides (p>0.05). C2, on the other hand, showed a statistically significant larger lamina diameter on the left side (mean±SD, 5.90±1.32 mm) compared with that on the right side (mean±SD, 5.59±1.27 mm; p=0.003) but longer lamina length on the right side (mean±SD, 25.23±2.59 mm) compared with that on the left side (mean±SD, 24.68±2.51 mm; p=0.006). However, screw acceptability between the right and left in C1 and C2 was similar (p=0.703 and p=0.243, respectively).
Discussion
Upper cervical fixation evolved from C1/C2 spinous process wiring, posterior C1/C2 interlaminar clamps, and a C1/C2 transarticular screw to the current C1 lateral mass screw method with a C2 pedicle screw construct. The aim was to achieve stability in fusion while avoiding complications such as vertebral artery injury, dural tearing, and neurologic injury [1,15,16]. According to a study done by Yeom et al. [3], the C2 vertebral artery groove violation was as high as 9.5% in the transarticular screw and 21% in the pedicle screw [4]. The risk of vertebral artery groove violation by the screw is higher when there is the presence of a narrow C2 pedicle and/or a high-riding vertebral artery, which are present in 22.83% and 10.1%–16.54% of patients, respectively [4,17,18].
The atlas translaminar (posterior arch) screw was initially introduced by Floyd and Grob [19] as a method of augmentation and to hold the bone graft. The atlas posterior arch screw was later utilized as a salvage method of fixation when the usual method of fixation was not feasible because of the presence of a tumor, unfused C1 posterior arch, high-riding vertebral artery, or an aberrant vertebral artery course [7,8,20,21]. The C1 and C2 laminar screw offers less risk of vertebral artery injury as the procedure is done under direct visualization [3,10,22,23]. However, care should be taken when inserting the laminar screw in C1, especially to not breach the superior cortex where the vertebral artery passes at the superior aspect in the vertebral artery groove [20].
Guo-Xin and Huan [10] performed a biomechanical study comparing a bilateral C1–C2 pedicle screw with a combination of a unilateral pedicle screw, a C1 posterior arch screw, and a C2 laminar screw. They found that both instances of construct movement were reduced compared with the control, and there was no significant difference in flexion–extension and rotation between the two constructs. However, a bilateral pedicle screw has better stability in terms of lateral bending [10]. Shen et al. [23] performed a similar biomechanical study with an additional crossed-rod construct between a pedicle and a laminar screw between C1 and C2. They found that all the constructs have similar stability in terms of flexion, extension, lateral bending, and axial rotation [23]. Cadena et al. [22] performed a different study comparing C1 lateral mass/C2 pars screw rod construct with the C1 posterior arch/C2 pars screw rod construct. They also found that both the constructs had reduced motion in the flexion–extension and axial rotation compared with the intact specimen, and the C1 lateral mass/C2 pars screw rod construct provided rigidity in lateral bending. However, there was no notable difference between the two constructs in flexion–extension, rotation, and lateral bending [22].
According to all the biomechanical studies done and previous case reports on successful fusion, we believe that the C1 and C2 laminar screw has the potential to be used as an additional construct for added stability or to even replace the current method of fixation due to its similar stability with less of a risk of neurovascular injury. Our CT morphometric analysis of C1 and C2 shows that it is feasible to use laminar screws in the Malay population in Malaysia, especially in males, and that this could be extrapolated to include the whole Malaysian population. This study also gives the surgeon a better understanding of the dimensions of C1 and C2, which will help in preoperative planning as well as in intraoperative selection of the method of fixation and screw sizes. A laminar screw would be a safer alternative for a patient with a high-riding vertebral artery [22], anomalous vertebral arteries [7,8], a unilateral occluded vertebral artery [8], lateral mass destruction of C1 or C2 by a tumor [20,21], or any other condition that makes the current existing method of fixation not feasible.
The criteria used for screw acceptability in our study is similar to those in previous studies, as we assumed a margin of error of 0.5 mm on each side for a 3.5-mm screw [7]. In our study, the mean bicortical diameter 5.79±1.19 mm and height 9.76±1.51 mm of C1 is similar to those of the study conducted by Yew et al. [7]. However, Yew et al. [7] reported a longer C1 lamina length of 24.21±2.85 mm on the right and 24.39±2.76 mm on the left compared with our study. This is attributed to the different method of measurement, as they measured from the midline to the lateral mass/lamina junction, which includes the vertebral artery groove in the measurement. Our study, on the other hand, measured the actual length according to the screw trajectory, from the entry point at the cortex up to the junction of the lamina and the most posterior edge of the vertebral artery groove, which excludes the vertebral artery groove from the measurement. Our study has a higher screw acceptance rate in terms of diameter and height compared with the study by Yew et al. [7], which reported 75.9% of lamina having a sufficient diameter and 63.7% of lamina having sufficient height for the screw. This might be attributed to the higher percentage of female subjects in their study (our study is skewed toward the male subject, 4.5:1 male-to-female ratio) as females are shown to have a lower screw acceptance rate. Overall, our study has a better assessment on screw acceptability as we assess each individual subject separately according to their parameters (diameter, height, and length) in combination, rather than looking at the general mean measurement.
Our study has a similar screw acceptability in a cross configuration in C1 as that of Xiang et al. [24] who performed CT morphometric analysis of C1 in the pediatric population and reported screw acceptability of 59.1% in subjects over 13 years old. The high screw acceptability in their study, although the pediatric population generally has smaller bone dimensions, may be attributed to the patients being near skeletal maturity and their lower screw acceptance criteria of a minimum 4 mm in diameter, 8 mm in height, and 15 mm in length.
Our study on C2 dimensions produced similar means across diameter, height, and length compared with previous studies [11,25]. We found that the majority of the population (80.3%) has a C2 lamina dimension that is able to accommodate a 3.5-mm laminar screw in a cross configuration, which is similar to previous studies [11,25-28].
The screw acceptability of the C1 lamina is 79.4% on the right and 78.2% on the left, with this being dropped to 65.5% in the bilateral cross screw, whereas the screw acceptability of the C2 lamina is over 80% whether it is a unilateral or bilateral cross screw. However, a higher percentage of the patients may be able to accommodate a laminar screw in view of the presence of viscoelastic accommodation. Both pediatric and adult pedicles have been proven to demonstrate viscoelastic circumferential expansion, enabling them to accept a screw much larger than their endosteal diameter [29]. Cahill et al. [30] reported that the pedicle can accommodate a screw that is 125 (14.6%) of the original external transverse diameter where the circumference generally increases by 4%. This viscoelastic accommodation properties of the pedicle should be present in the lamina as well. However, new studies are required to determine the degree of lamina expansion prior to cortical failure [11].
A higher percentage of bilateral screw acceptability will also be achieved if screws are placed according to Donnellan et al. [20] as their screw construct does not cross at the midline. Therefore, the required lamina height will only be 4.5 mm instead of 9.0 mm, and a screw can be inserted in patients with an incomplete fusion of the C1 posterior arch [20]. However, this screw construct will produce a shorter lamina for screw placement, therefore reducing the stability and pull-out strength.
According to our study, the C1 lamina has a mean length of 20.70 mm with a range of 11.70 to 25.80 mm, and the C2 lamina has a mean length of 24.96 mm with a range of 16.40 to 35.40 mm. The lamina of C2 is generally longer than that of C1, as it is not limited by the vertebral artery groove. The reported laminar screws that are used range from 14 to 22 mm [10,21,23]. Riesenburger et al. [9] found that the C2 laminar screw, if limited to 28 mm in length, is safe. However, there are limited studies on optimum screw length that can provide adequate stability and pull-out strength while being in the safe zone inside the lamina. Therefore, a preoperative CT scan should be performed to assess the lamina dimension for screw feasibility and to estimate the screw length.
There are a number of limitations to our study. First, our sample is skewed toward male patients, which may result in the slightly larger mean value of parameters. Second, measurement error is unavoidable. Third, this study is limited to the Malaysia Malay population, and the results might not be able to be extended to other ethnic groups. Last, this is only a CT morphometric study without actual clinical application during the study.
Conclusions
Our study found that it is feasible to insert a 3.5-mm screw in a cross configuration in the C1 and C2 laminas of Malaysian Malay patients, especially in males. A laminar screw can be used as a method of fixation or used in combination with another construct to increase stability while providing a safer and less technically demanding option. However, more biomechanical study should be done, comparing different screw sizes and length and different combinations of the construct with the aim to look for the construct that provides the best stability and also the optimum screw diameter and length that provides the best pull-out strength and rigidity. A CT scan must be done prior to an operation to identify patients that are suitable and to estimate the screw sizes; however, this study confirms the feasibility of this fixation technique in most of the patients in our population.
Notes
No potential conflict of interest relevant to this article was reported.