Postoperative Low Back Pain after Posterior Lumbar Interbody Fusion Surgery Using Cortical Bone Trajectory Screws
Article information
Abstract
Study Design
Retrospective analysis of a case series of prospectively collected data.
Purpose
To compare clinical and radiological outcomes between two posterior lumbar interbody fusion techniques: cortical bone trajectory (CBT) and traditional pedicle screw (PS).
Overview of Literature
Biomechanical studies have revealed the benefits of the CBT technique. However, clinical evidence obtained from the direct comparison of outcomes between CBT and PS is limited.
Methods
We retrospectively investigated 104 patients who had undergone posterior lumbar interbody fusion using CBT or PS. Clinical symptoms were evaluated and compared between CBT and PS using the Japanese Orthopedic Association Back Pain Evaluation Questionnaire (JOABPEQ) and Visual Analog Scale (VAS) before and 1 year after surgery. Spinal fusion status was assessed by multiplanar reconstruction computed tomography at 1 year after surgery.
Results
The CBT and PS techniques were performed on 36 and 68 patients, respectively. Both CBT- and PS-treated patients exhibited improvement in each subdomain of the JOABPEQ and in the VAS. With regard to postoperative improvement of low back pain, the treatment effect, as assessed by the JOABPEQ, was greater for PS than for CBT. The spinal fusion rate was slightly lower for CBT than for PS, although the difference between them was not significant. The effect of treatment on postoperative low back pain was smaller for CBT than for PS, regardless of whether rigid spinal fusion was achieved.
Conclusions
Clinical symptoms and spinal fusion efficiency were not significantly different between CBT and PS except for postoperative improvement in low back pain. The treatment effect on postoperative low back pain was smaller for CBT than for PS.
Introduction
Posterior lumbar interbody fusion (PLIF) is widely used to treat degenerative lumbar disorders. PLIF tends to be combined with the use of a pedicle screw (PS) system. The cortical bone trajectory (CBT) technique is a novel PS method that was advocated by Santoni et al. [1]. Theoretically, CBT provides increased bone purchase and is thought to improve initial fixation by optimizing the contact of the screw with the cortical bone of the vertebrae [2]. In CBT, the screws are placed in a medial-to-lateral direction along a caudo-cephalad path, with the objective of maximizing thread contact with higher-density bone. In addition, the medial entry of the screw in CBT allows for less soft tissue dissection than that associated with the use of traditional PSs. Therefore, patients treated with CBT are expected to have less postoperative pain because of the smaller incision and decreased disruption of muscle attachments.
CBT appears to have several advantages over PS. However, clinical evidence that directly compares outcomes and complications between CBT and PS is limited. Most reports have described no significant differences in postoperative back or leg pain between patients who have undergone CBT and PS [3-6].
This study was performed to compare clinical and radiological outcomes in terms of postoperative pain, function, and bony fusion status between the CBT technique and the traditional PS technique. We performed PLIF for the treatment of degenerative lumbar disorders using either the CBT or PS technique and examined the surgical outcomes.
Materials and Methods
A total of 172 patients with lumbar degenerative disease and instability underwent PLIF between 2014 and 2017 at Osaka General Medical Center, Osaka, Japan. This study has been reviewed and approved by the institutional review board of Osaka General Medical Center (24-2015). Informed consent was obtained from all patients included in this study. We performed the PS technique on Wednesdays and the CBT technique on Fridays. Two experienced spine surgeons performed the CBT and PS surgeries. We excluded patients who were undergoing treatment with either dialysis (n=3) or corticosteroids (n=14). We also excluded patients who had undergone PLIF at more than two levels (n=22, including one with dialysis and two with corticosteroids) or PLIF in the L5/S region (n=34, including two with corticosteroids). The remaining 104 patients were included, and their data were retrospectively analyzed.
CBT screws were inserted based on the method described by Santoni et al. [1]. We decided to use the longest possible screws in order to increase fixation strength, as suggested elsewhere [7]. The mean screw length was 39.4 mm for CBT and 44.9 mm for PS. Both CBT and PS surgeries were performed using the MAS (Maximum Access Surgery) PLIF system screws and a CoRoent polyetheretherketone cage (NuVasive Inc., San Diego, CA, USA). Within 1 week after surgery, multiplanar reconstruction computed tomography (CT) was performed to evaluate the screw positioning in all patients. Medical records and CT findings were reviewed to identify complications, including dural tear, pedicle fracture, epidural hematoma, and surgical site infection, that occurred within 30 days postoperatively. All patients used a lumbosacral orthosis for 3 months after surgery.
Clinical symptoms were evaluated before and 1 year after surgery using the 100-point Japanese Orthopedic Association Back Pain Evaluation Questionnaire (JOABPEQ; 0=worst, 100=best) and the 10-point Visual Analog Scale (VAS; 0=no pain, 10=worst pain imaginable) [8]. The JOABPEQ was developed based on the Roland-Morris Disability Questionnaire and the 36-item Short Form Health Survey. The postoperative changes in each of the five subdomains of the JOABPEQ (low back pain, lumbar function, walking ability, social life function, and mental health) were calculated based on the preoperative scores. VAS scores (low back pain, pain in the buttocks and lower limbs, and numbness in the buttocks and lower limbs) were also recorded before and 1 year after surgery.
We assessed spinal fusion status by CT 1 year after surgery. Spinal fusion was determined by the continuity of bone trabeculae between the vertebra and the grafted bone [9].
The unpaired t-test, Mann-Whitney U-test, Wilcoxon signed-rank test, Kruskal-Wallis test, and Fisher’s exact probability test were used for statistical analysis as appropriate. All p-values of <0.05 were considered statistically significant. All statistical analyses were performed with EZR (Saitama Medical Center, Jichi Medical University, Saitama, Japan), which is a graphical user interface for R ver. 2.3.0 (The R Foundation for Statistical Computing, Vienna, Austria). More precisely, it is a modified version of R Commander designed to add statistical functions that are frequently used in biostatistics [10].
Results
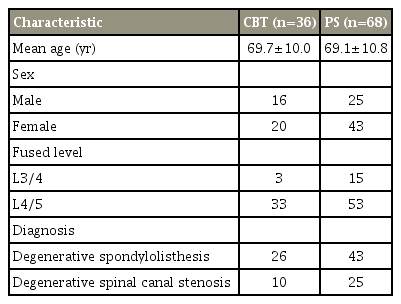
The CBT and PS techniques were performed on 36 and 68 patients, respectively (Table 1, Fig. 1). The patients comprised 41 men and 63 women. The mean age at surgery was 69.3 years (CBT, 69.7 years; PS, 69.1 years). The diagnosis at the time of surgery was degenerative spondylolisthesis in 69 patients and degenerative spinal canal stenosis in 35 patients. The mean estimated intraoperative blood loss volume in the overall study population was 239±106 mL (247±106 mL in CBT-treated patients; 235±108 mL in PS-treated patients). The spinal fusion was performed at L3/4 in 18 patients and at L4/5 in 86 patients.
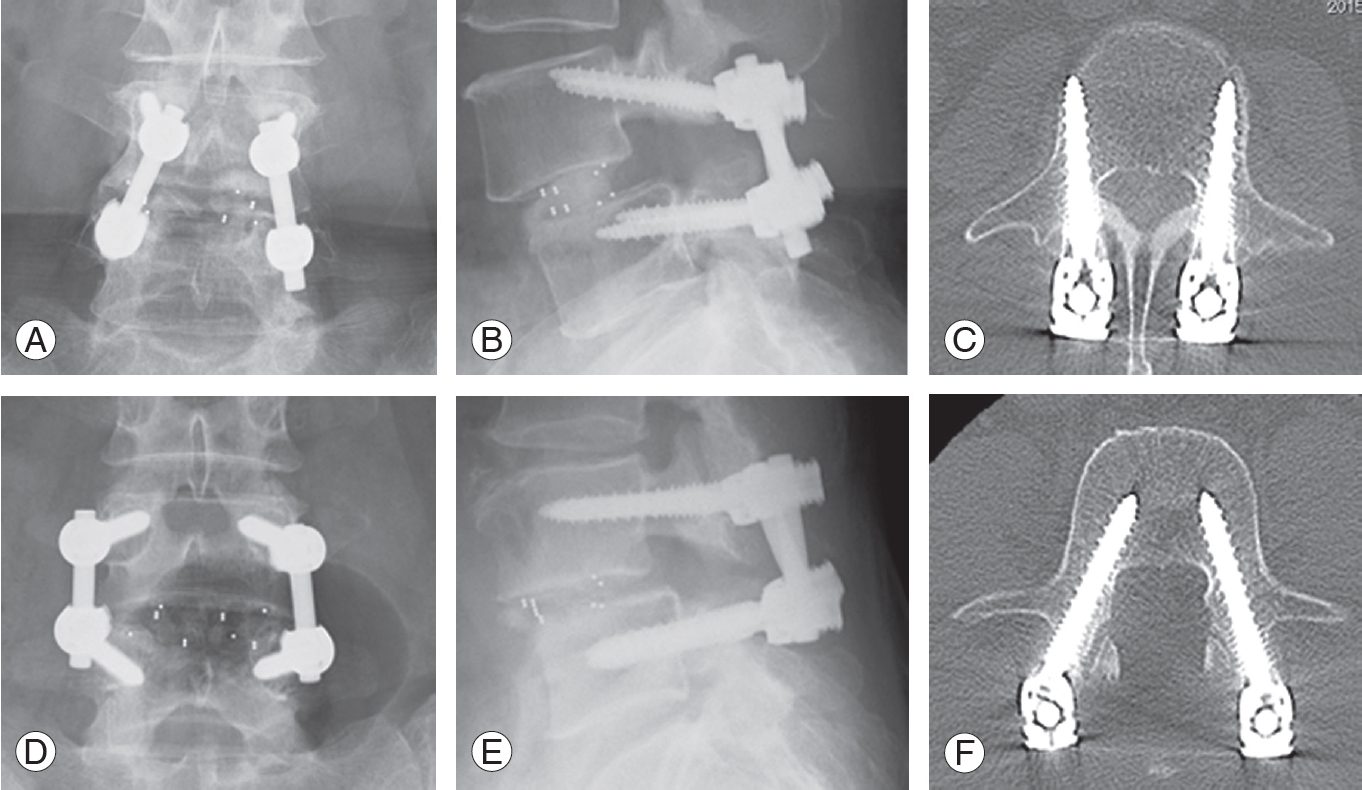
Representative radiographs and CT images of the CBT and PS techniques. (A) Anteroposterior radiograph, (B) lateral radiograph, and (C) CT image of the CBT technique. (D) Anteroposterior radiograph, (E) lateral radiograph, and (F) CT image of the PS technique. CT, computed tomography; CBT, cortical bone trajectory; PS, pedicle screw.
Both CBT- and PS-treated patients exhibited improvement in all subdomains of the JOABPEQ after PLIF (Fig. 2). There was no significant difference in the JOABPEQ scores between the CBT- and PS-treated patients except for low back pain improvement. Although low back pain improved in patients who underwent CBT, the treatment effect was smaller than that in patients who underwent PS (CBT, 11.7 points; PS, 28.9 points; p=0.04). VAS scores similarly improved after PLIF but with no significant difference between CBT and PS in each domain (Fig. 3). Compared with patients who underwent PS, those who underwent CBT had less improvement of low back pain associated with both degenerative spondylolisthesis and degenerative spinal canal stenosis.

JOABPEQ scores before and 1 year after surgery. (A) Low back pain. (B) Lumbar function. (C) Walking ability. (D) Social life function. (E) Mental health. 100-point scale: 0=worst, 100=best. CBT, cortical bone trajectory; PS, pedicle screw; Pre, presurgery; 1 yr, 1 year after surgery; JOABPEQ, Japanese Orthopedic Association Back Pain Evaluation Questionnaire. *p<0.05.

VAS scores before and after surgery. (A) Low back pain. (B) Pain in the buttock and lower limb. (C) Numbness in the buttock and lower limb. 10-point scale: 0=no pain, 10=worst pain imaginable. CBT, cortical bone trajectory; PS, pedicle screw; Pre, pre-surgery; 1 yr, 1 year after surgery; VAS, Visual Analog Scale.
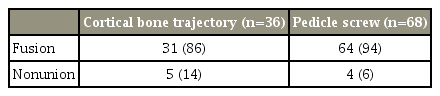
The spinal fusion rate of CBT was slightly lower than that of PS (Table 2). Spinal fusion was achieved in 86% of CBT-treated patients and in 94% of PS-treated patients. There was no significant difference between the two groups.
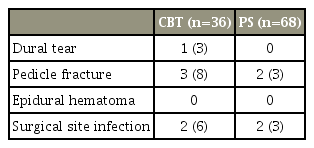
Perioperative complications are summarized in Table 3. Pedicle fracture occurred in three CBT-treated patients (8%) and two PS-treated patients (3%). All pedicle fractures were healed without screw loosening at 1 year postoperatively. Spinal fusion was achieved in all PS-treated patients and in all but one CBT-treated patient. These pedicle fractures did not cause any clinical symptoms.
The effect of surgical treatment on low back pain was smaller in CBT-treated patients, regardless of spinal fusion status (Fig. 4). Because postoperative low back pain is associated with nonunion after spinal fusion surgeries [11], we re-evaluated this clinical symptom in patients who had achieved solid spinal fusion (CBT, n=31; PS, n=64). The improvement in postoperative low back pain was still smaller with CBT than with PS (p=0.04).
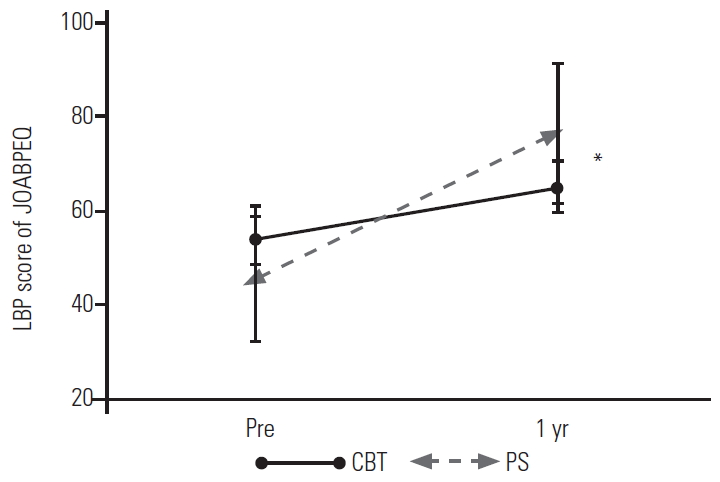
LBP score of JOABPEQ before and after surgery with patients who achieved spinal fusion. 100-point scale: 0=worst, 100=best. CBT, cortical bone trajectory; PS, pedicle screw; Pre, pre-surgery; 1 yr, 1 year after surgery; LBP, low back pain; JOABPEQ, Japanese Orthopedic Association Back Pain Evaluation Questionnaire. *p<0.05.
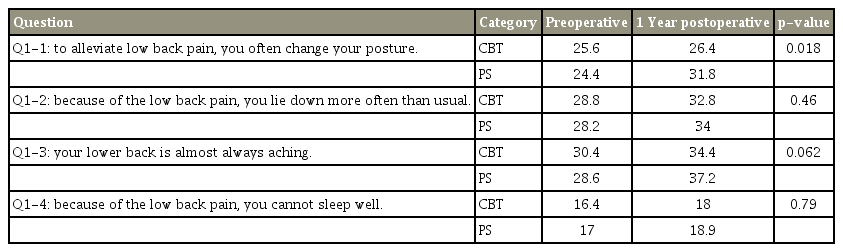
There was a moderate discrepancy in postoperative low back pain improvement as assessed using the JOABPEQ versus the VAS. The JOABPEQ score for low back pain consists of four questions. The score for question 1-1 differed significantly between CBT- and PS-treated patients (Table 4). Patients treated by PS demonstrated significantly greater improvement with regard to the need to change their posture in order to alleviate low back pain.
Discussion
With the exception of postoperative improvement in low back pain, the clinical results and spinal fusion rate did not differ significantly between CBT and traditional PS.
In the subclinical domain of low back pain in the JOABPEQ, patients treated with CBT showed less improvement than patients treated with PS. Most studies have demonstrated no clinical difference between CBT and PS, including in terms of postoperative low back pain [3-6]. CBT is believed to have an advantage in terms of postoperative pain because of its smaller incision and reduced muscle dissection. However, one report described the deterioration of postoperative pain at 6 to 8 months of follow-up in CBT-treated patients [12]. In the present study, low back pain as measured by the VAS similarly exhibited less postoperative improvement with CBT than with PS; however, the difference was not statistically significant. The JOABPEQ score for low back pain consists of four questions and measures low back pain as related to quality of life and general well-being [13], which is different from the low back pain measurement of the VAS.
The spinal fusion rate of CBT-treated patients was slightly lower than that of PS-treated patients, which is consistent with previous studies [3,14]. A cadaveric biomechanical study using a low-bone-quality model demonstrated that standard PS exhibited better fatigue performance than CBT screws [15]. Another biomechanical study revealed that traditional PS fixation is stiffer than CBT screw fixation during axial rotation and lateral bending [16]. Thus, micromotion in CBT-treated patients might result in a lower rate of spinal fusion than that in PS-treated patients. In addition, the fixation strength of CBT screws varied depending on screw size [7]. The ideal diameter and length for a CBT screw are reportedly >5.5 mm and >35 mm, respectively, which allows the screw to be placed sufficiently deep into the vertebral body. Although we used the longest possible screws (mean length, 39.4 mm), the spinal fusion rate of CBT was slightly lower than that of PS.
Pedicle fracture is a frequent complication of the CBT technique, with an incidence of around 4% [6,17,18]. As the CBT technique allows the screw to engage the denser regions, there is a potential risk of pedicle fracture during screw insertion. In our study, pedicle fractures were observed in 8% of CBT-treated patients; however, these pedicle fractures did not affect either spinal fusion or postoperative low back pain.
CBT-treated patients exhibited less improvement in low back pain than PS-treated patients, despite the achievement of solid spinal fusion. Postoperative low back pain has been associated with nonunion after spinal fusion surgery [11]. Although we re-examined clinical symptoms only in patients with solid spinal fusion, the degree of improvement in postoperative low back pain was still smaller in CBT-treated patients than in PS-treated patients.
All four questions in the JOABPEQ concerning low back pain tended to reflect better results in PS-treated patients than in CBT-treated patients. In particular, there was a significant difference between PS- versus CBT-treated patients regarding the question “to alleviate low back pain, you often change your posture.” It is not clear what this result indicates. CBT surgeries usually involve a small skin incision. Back muscle retraction through this small skin incision increases the intramuscular pressure to a level that impedes local blood flow of the muscle and leads to muscle degeneration [19,20]. Postoperative magnetic resonance imaging demonstrated that the CBT screw head replaced the multifidus because of the screw’s medial-to-lateral orientation and caudo-cephalad pathway (Fig. 5). Muscle retraction due to the small skin incision or screw head irritation against the multifidus might cause back muscle damage, resulting in insufficient improvement in low back pain.

Representative postoperative magnetic resonance imaging for (A) cortical bone trajectory technique and (B) pedicle screw technique. Degeneration of the multifidus (arrow) was observed after cortical bone trajectory surgery.
The present study has some limitations. First, we randomly assigned patients to undergo either the CBT or PS technique without evaluating their bone mineral density. As the CBT technique is expected to improve the adhesion of screws in osteoporotic vertebrae, the CBT technique might have exhibited better results than the PS technique if the present study had been limited to osteoporotic patients. Second, our evaluations were only performed before surgery and at 1 year after surgery. CBT-treated patients might exhibit better improvement in low back pain in the early postoperative period than PS-treated patients, as the CBT technique is less invasive than the PS technique. Third, low back pain could be associated with factors other than spinal canal stenosis or spondylolisthesis, such as lumbar disc degeneration [21], which would not be improved by surgical treatment.
Conclusions
Except for postoperative improvement in low back pain, the clinical symptoms and spinal fusion efficiency were not significantly different between CBT and PS. The treatment effect on postoperative low back pain was smaller for CBT than PS.
Notes
No potential conflict of interest relevant to this article was reported.
Author Contributions
NN and HK designed the study and wrote the manuscript. NN, TM, and HK performed the experiment.
Acknowledgements
We thank Angela Morben, DVM, ELS, from Edanz Group (www.edanzediting.com/ac), for editing a draft of this manuscript.