3. Linton SJ. Occupational psychological factors increase the risk for back pain: a systematic review. J Occup Rehabil 2001 11:53–66.


4. Trinkoff AM, Lipscomb JA, Geiger-Brown J, Brady B. Musculoskeletal problems of the neck, shoulder, and back and functional consequences in nurses. Am J Ind Med 2002 41:170–8.


5. Smith DR, Kondo N, Tanaka E, Tanaka H, Hirasawa K, Yamagata Z. Musculoskeletal disorders among hospital nurses in rural Japan. Rural Remote Health 2003 3:241.


6. Shieh SH, Sung FC, Su CH, Tsai Y, Hsieh VC. Increased low back pain risk in nurses with high workload for patient care: a questionnaire survey. Taiwan J Obstet Gynecol 2016 55:525–9.


8. Samaei SE, Mostafaee M, Jafarpoor H, Hosseinabadi MB. Effects of patient-handling and individual factors on the prevalence of low back pain among nursing personnel. Work 2017 56:551–61.


10. Zhuang Z, Stobbe TJ, Hsiao H, Collins JW, Hobbs GR. Biomechanical evaluation of assistive devices for transferring residents. Appl Ergon 1999 30:285–94.


11. Peterson EL, McGlothlin JD, Blue CL. The development of an ergonomics training program to identify, evaluate, and control musculoskeletal disorders among nursing assistants at a state-run veterans’ home. J Occup Environ Hyg 2004 1:D10–6.


12. Humphreys SL. Obesity in patients and nurses increases the nurse’s risk of injury lifting patients. Bariatr Nurs Surg Patient Care 2007 2:3–6.

13. Kubota S, Nakata Y, Eguchi K, et al. Feasibility of rehabilitation training with a newly developed wearable robot for patients with limited mobility. Arch Phys Med Rehabil 2013 94:1080–7.


15. Kubota S, Kadone H, Shimizu Y, et al. Robotic rehabilitation training with a newly developed upper limb single-joint Hybrid Assistive Limb (HAL-SJ) for elbow flexor reconstruction after brachial plexus injury: a report of two cases. J Orthop Surg (Hong Kong) 2018 26:2309499018777887.


16. Hara H, Sankai Y. Development of HAL for lumbar support. In: Proceedings of the SCIS and ISIS 2010: Joint 5th International Conference on Soft Computing and Intelligent Systems and 11th International Symposium on Advanced Intelligent Systems; 2010 Dec 8-12; Okayama, Japan. Okayama: Committee of SCIS-ISIS. 2010 416–21.
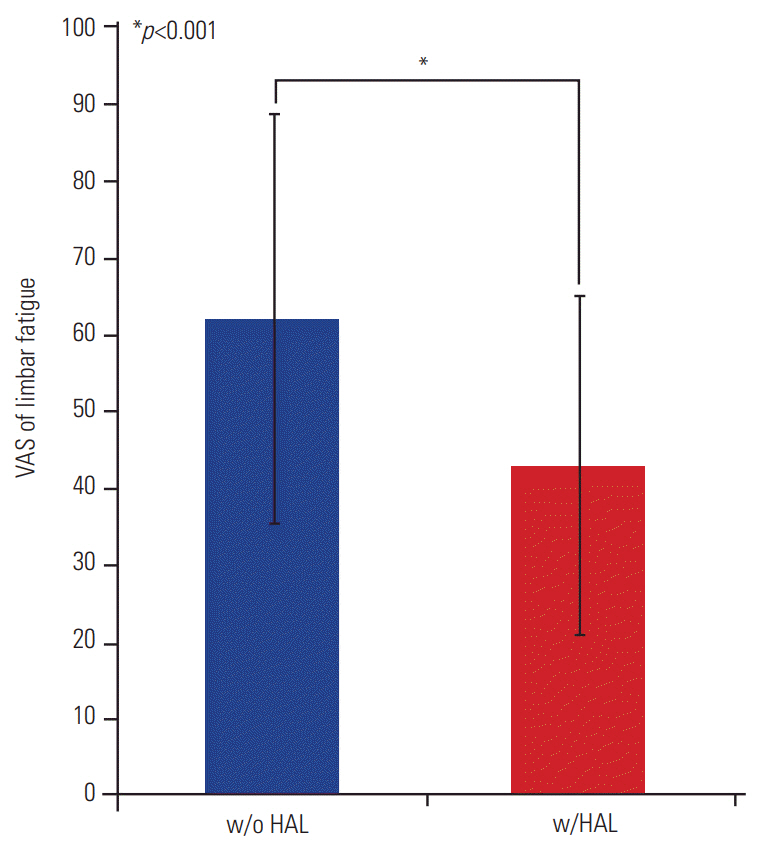
17. Miura K, Kadone H, Koda M, et al. The hybrid assisted limb (HAL) for Care Support, a motion assisting robot providing exoskeletal lumbar support, can potentially reduce lumbar load in repetitive snowshoveling movements. J Clin Neurosci 2018 49:83–6.


18. Miura K, Kadone H, Koda M, et al. The hybrid assistive limb (HAL) for Care Support successfully reduced lumbar load in repetitive lifting movements. J Clin Neurosci 2018 53:276–9.


19. Hignett S. Work-related back pain in nurses. J Adv Nurs 1996 23:1238–46.


21. Lorusso A, Bruno S, L’Abbate N. A review of low back pain and musculoskeletal disorders among Italian nursing personnel. Ind Health 2007 45:637–44.


22. Choi SD, Brings K. Work-related musculoskeletal risks associated with nurses and nursing assistants handling overweight and obese patients: a literature review. Work 2015 53:439–48.


23. Marras WS, Davis KG, Kirking BC, Bertsche PK. A comprehensive analysis of low-back disorder risk and spinal loading during the transferring and repositioning of patients using different techniques. Ergonomics 1999 42:904–26.


24. Hegewald J, Berge W, Heinrich P, et al. Do technical aids for patient handling prevent musculoskeletal complaints in health care workers?: a systematic review of intervention studies. Int J Environ Res Public Health 2018 15:E476.

25. Richardson A, McNoe B, Derrett S, Harcombe H. Interventions to prevent and reduce the impact of musculoskeletal injuries among nurses: a systematic review. Int J Nurs Stud 2018 82:58–67.


26. Van Hoof W, O’Sullivan K, O’Keeffe M, Verschueren S, O’Sullivan P, Dankaerts W. The efficacy of interventions for low back pain in nurses: a systematic review. Int J Nurs Stud 2018 77:222–31.