Surgical Outcomes and Correlation of the Copenhagen Neck Functional Disability Scale and Modified Japanese Orthopedic Association Assessment Scales in Patients with Cervical Spondylotic Myelopathy
Article information
Abstract
Study Design
Cross-sectional.
Purpose
Clinical outcome study comparing the Copenhagen Neck Functional Disability Scale (CNFDS) and modified Japanese orthopedic association (mJOA) assessment scales in patients with cervical spondylotic myelopathy (CSM).
Overview of Literature
Comparison of instruments that measure patient-reported outcomes is needed.
Methods
A cross-sectional analysis was conducted. Ninety five patients with CSM were entered into the study and completed the CNFDS and the mJOA preoperatively and postoperatively. Correlation between the CNFDS and the mJOA was evaluated preoperatively and at the end of follow-up. Responsiveness to change of CNFDS and mJOA was also assessed. Clinical outcomes were also measured with the recovery rate of mJOA score at end of follow-up.
Results
The mean age of patients was 58.2 (standard deviation, SD=8.7) years. Mean follow-up was 2.1 years (range, 1 to 4 years). The mJOA correlated strongly with the CNFDS score preoperatively and postoperatively (r=–0.81 and –0.82, respectively; p<0.001). The CNFDS and the mJOA were able to detect changes after the surgery (p<0.001). The mean mJOA recovery rate was 51.8% (SD=13.1%).
Conclusions
Surgery for the treatment of patients with CSM is an efficacious procedure. CNFDS and mJOA scores have a strong correlation in measuring disability among CSM patients.
Introduction
Cervical spondylotic myelopathy (CSM) refers to the impaired function of the spinal cord caused by degenerative changes of the discs and facet joints in the cervical spine. It includes cervical herniated disc (CHD) and cervical spinal stenosis (CSS), and is a progressive spine disease. CSM symptoms depend on the level(s) of the spinal cord involvement and its pattern [1].
The variety of measures to evaluate CSM and disability for clinical or research purposes include the neck disability index (NDI) [2], northwick park neck pain questionnaire [3], Copenhagen Neck Functional Disability Scale (CNFDS) [4], neck pain and disability scale (NPAD) [5], Bournemouth questionnaire for neck pain (BQN) [6], patient-specific functional scale [7], modified Japanese Orthopedic Association (mJOA) criteria [89], Japanese Orthopaedic Association Cervical Myelopathy Evaluation Questionnaire (JOACMEQ) [10], Nurick-score [1112], Japanese Orthopaedic Association (JOA) score [13], Cooper-myelopathy-scale [14], Proloscore [15], European-myelopathy-score [16] and the CNFDS [17]. However, it is argued that none of these measures can be considered as a golden standard [1518]. In addition, each measure has advantages and disadvantages.
This paper explores the use of the CNFDS and the mJOA tools that have been validated for specific conditions. It is unclear whether these two functional scoring systems provide similar evaluations of patients with CSM. Hence, the purpose of this study was surgical outcome assessment and to determine the correlation between the CNFDS and the mJOA scales before and after surgery in patients with CSM.
Materials and Methods
1. Patients and data collection
The final draft of the Iranian versions of the CNFDS and mJOA were administered to a sample of newly diagnosed CSM patients attending the neurosurgery clinic of a large teaching hospital in Tehran, from April 2007 to June 2013. CSM was diagnosed on the basis of appropriate history, clinical examination, and investigations, notably magnetic resonance imaging or computed tomography (CT) scan of the cervical spine. There were no restrictions on patient selection with regard to types of CSM, age or other characteristics. The exclusion criteria were prior cervical spine surgery or other coexisting pathology that might result in functional impairment. All patients had the typical symptoms of CSM and were surgical candidates.
2. Surgery procedure
The key to the treatment of the CSM is to remove the pressure from the spinal cord. Surgical methods to decompress the spinal cord included three approaches: (1) from the front of the neck as anterior cervical discectomy and fusion, anterior cervical corpectomy, and (2) from the back of the neck as cervical laminectomy, cervical laminectomy and fusion, cervical laminoplasty, and (3) a combined procedure [19]. All three approaches were applied to the patients.
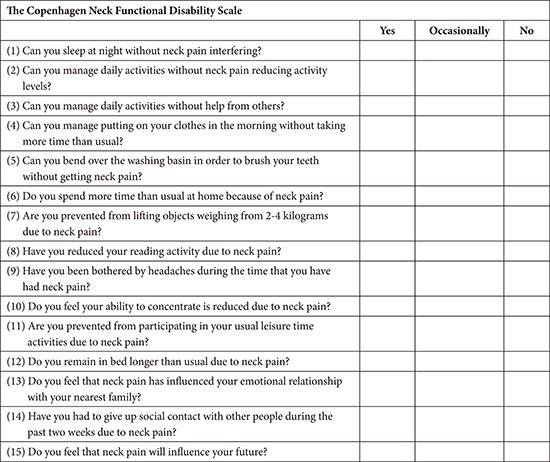
3. CNFDS
The CNFDS (Appendix 1) is designed to evaluate the disability experienced by CSM patients. It is a self-administered questionnaire that consists of three sections including 15 items that evaluates the impact of neck pain including the patient's perception of the future impact of neck pain (3 items including 1, 5, and 15), disability during everyday activities (9 items including items 2, 3, 4, 5, 7, 8, 9, 10 and 12) and social interaction and recreation (5 items including item 6, 9, 11, 13 and 14). Each item has three possible response categories (yes=0, occasionally=1 and no=2) for the first 5 items and the remaining items are scored in the reverse (yes=2, occasionally=1 and no=0). The total score ranges from 0 to 30, with higher score indicating greater disability [17].
4. mJOA
The Iranian version of the mJOA was simultaneously administered to patients. It is a self-administered, disease-specific tool modified from the JOA score [89] that consists of four sections including 22 items: motor dysfunction of the upper extremities (6 items), motor dysfunction of the lower extremities (8 items), sensation (4 items) and sphincter dysfunction (4 items). The score the respective section ranges from 0 to 5, 0 to 7, 0 to 3 and 0 to 3, giving a total score ranging from 0 to 18. Higher scores indicate less disability. In this study the total mJOA was calculated for assessment. In a previous study by this group, the Iranian version of mJOA was documented as a reliable and valid measure of motor, sensory and sphincter dysfunctions among CSM patients [9].
Patients were assessed preoperatively and postoperatively. CNFDS and mJOA scoring were completed at the same time on the day before surgery and at the end of follow-up. The recovery rate of mJOA score (%) was also assessed using a previously published formula [20]: recovery rate (%)=[postoperative score–preoperative score]/[full score (18)–preoperative score]×100.
5. Statistical analyses
Statistical analyses were performed using PASW ver. 18.0 (SPSS Inc., Chicago, IL, USA). A p-value of <0.05 was considered statistically significant. Correlation between the CNFDS and the mJOA was assessed using Pearson's correlation coefficient. Values of 0.40 or above were considered satisfactory (r≥0.81–1.0 as excellent, 0.61–0.80 very good, 0.41–0.60 good, 0.21–0.40 fair, and 0.0–0.20 poor) [21]. CNFDS and the mJOA scores were calculated preoperatively and postoperatively using the paired t-test to capture the changes after surgery.
6. Ethics
The Ethics Committee of Shahid Beheshti University of Medical Sciences, Tehran, Iran, approved the study.
Results
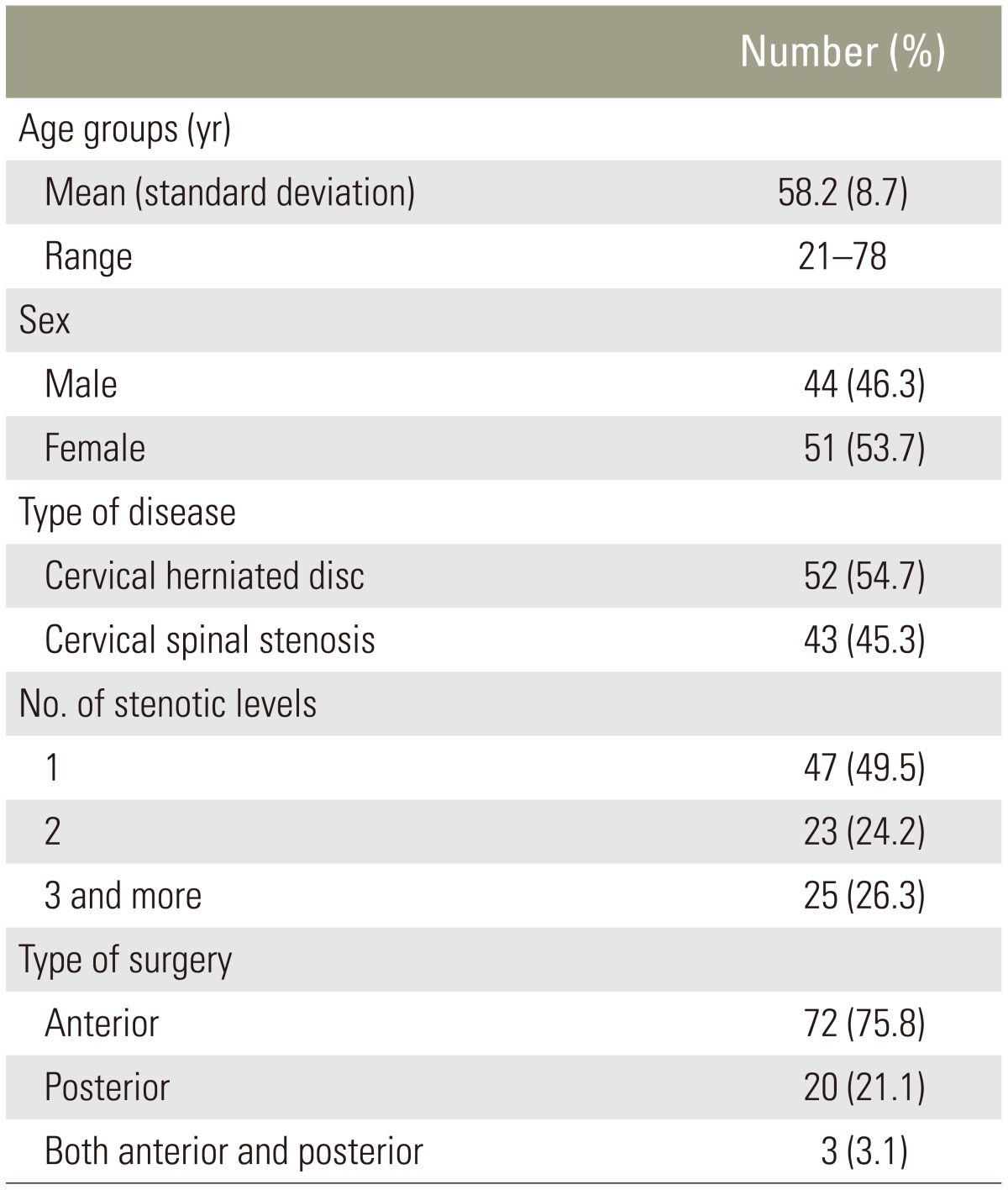
1. Study sample
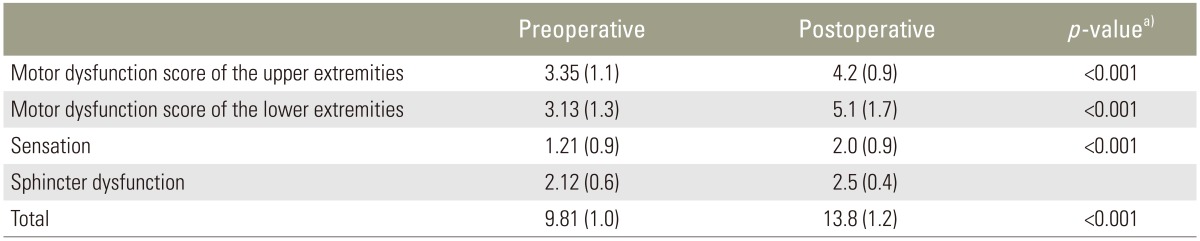
Ninety five patients with CSM were studied. Their mean age was 58.2 (standard deviation, SD=8.7) years. The mean symptom duration was 11.6 months (range, 1 to 59 months). The characteristics of patients and their scores on the mJOA are presented in Table 1. Most patients with CSM had a developmental narrow spinal canal, and the decompressive laminae were distributed from C2 to C7 levels. The number of decompressed lamina was 2.6 (SD=1.0). Most patients with CHD had a one- or two level discectomy and were distributed from the C2 to C7 levels. The anterior approach (discectomy/corpectomy with instrumented fusion; n=72), posterior approach (either laminectomy and fusion or laminoplasty; n=20), and combination of both anterior and posterior approaches (n=3) were performed for decompressive spinal surgery. Statistically differences were observed preoperative and postoperative assessments indicating improvements in outcomes and functionality in all subscales (p<0.001). However, there was no significant difference between patients with CSS and CHD (p≥0.05).
CNFDS total score correlated strongly with mJOA total score preoperatively and at the end of follow-up, lending support to its good convergent validity (r=–0.81 and –0.82, respectively; p<0.001) (Fig. 1). In all instances, CNFDS and mJOA tools were able to detect changes after the intervention (surgery), indicating improvements in all subscales. The outcomes are shown in Tables 2 and 3. The mean mJOA recovery rate was 51.8% (SD=13.1%), ranging from 23.0% to 88.8%.
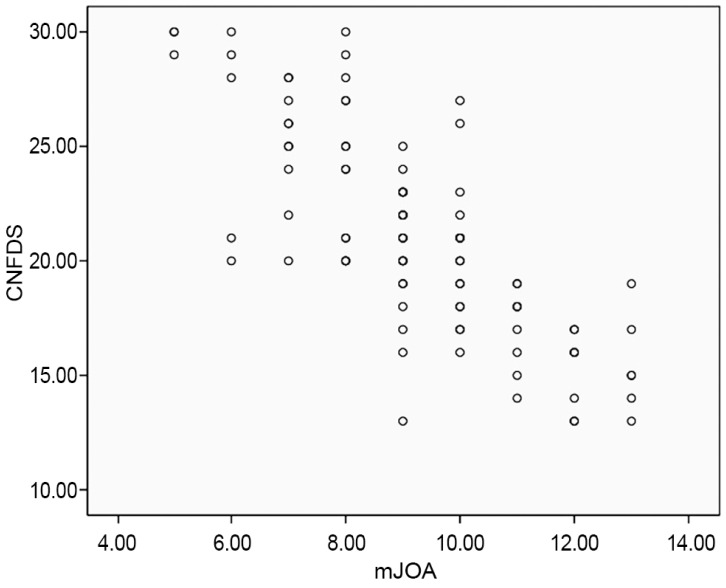
Total score of the Copenhagen neck functional disability scale (CNFDS) correlates strongly with total score of the modified Japanese orthopedic association (mJOA) preoperatively.
Discussion
This is the first report to measure disability in patients with CSM according to CNFDS and mJOA score with at least one year follow-up. The findings suggest that surgery for the treatment of patients with CSM is an efficacious procedure. It also indicates that the CNFDS and the mJOA tools have a strong correlation in measuring disability in patients with CSM at least one year follow-up.
Several authors reported clinical outcomes of decompressive surgery using the mJOA or the CNFDS score with a diverse range of research with successful outcome [1718222324252627], which is in line with our findings. Clinical outcomes, such as modified JOA recovery rate, were assessed [28]; the mean mJOA recovery rate was 50.7%±15.1% in elderly patients and 55.9±14.8 in non-elderly patients one year after surgery, with no statistically significant differences evident between the two groups. The present results are similar.
Few studies have compared Nurick grading and mJOA score in evaluating functional disability and outcome in patients with CSM [15]. The studies assessed the correlation in a small number of cases or in patients undergoing different types of decompressive surgery [29]. They reported that the mJOA could be utilized in assessment of these patients. However, to the authors' best knowledge, relations between the mJOA score and the CNFDS score have not been studied before.
To evaluate CSM and disability for clinical or research purposes, a variety of measures can be used including the mJOA, and the JOACMEQ. The mJOA and the CNFDS score can be used to assess of patients with CSM. However, none of these instruments can be considered as a golden standard [17]. Accordingly, to identify ways to improve care, we need more specific measures for patient assessment. Additional research is needed to assess the discriminant power of the tools for specific diagnostic entities.
This study had some limitations. The sample size was small, and the follow-up period was short. More studies are recommended. For assessment of CSM, Kalsi-Ryan et al. [30] reviewed related articles to identify the most suitable measurement of the scoring systems as mJOA for CSM. They pointed out that these measurements do not objectively quantify the physical findings of the individual. In addition, they suggested that clinicians can obtain more reliable and quantitative information in the CSM population using ancillary measurements, such as the 30-meter walk test [30]. JOA recovery rate is a simple and useful parameter to compare clinical outcomes quantitatively. However, JOA recovery rate is not the gold standard and the use of this score may be unreasonable [28]. Finally, it is not clear that difference in preoperative and postoperative scores is an appropriate approach for clinical outcomes. Hence, there is a need to establish the definitive standard for assessment of clinical outcomes in patients with CSM.
Conclusions
Surgery for the treatment of patients with CSM is an efficacious procedure. CNFDS and the mJOA scores have a strong correlation in measuring disability among CSM patients. Disease-specific tools like the mJOA and the CNFDS could be used in the assessment of patients with CSM.
Acknowledgments
The authors thank the staff of the Neurosurgery Unit Imam-Hossain Hospital, Tehran, Iran.
Notes
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
Appendices
Appendix 1
The Copenhagen Neck Functional Disability Scale.