Minimum 2-Year Experience with Magnetically Controlled Growing Rods for the Treatment of Early-Onset Scoliosis: A Systematic Review
Article information
Abstract
Magnetically controlled growing rods have been used to treat early-onset scoliosis for the last 9 years; however, few studies have been published, with only short-term follow-up. The aim of the present study is to systematically review the outcomes of magnetically controlled growing rods in the treatment of early-onset scoliosis with a minimum of 2-year follow-up. Studies were included if patients with early-onset scoliosis (scoliosis diagnosed before 10 years of age) underwent implantation of magnetically controlled growing rods with a minimum of 2-year follow-up. The literature review and data extraction followed the established preferred reporting items for systematic review and meta-analysis guidelines. Data of distraction frequency, number of distractions, distracted length, Cobb angle, kyphosis, T1–T12 length, and T1–S1 length preoperatively, postoperatively, and at final follow-up were collected. Data regarding complications and unplanned reoperations were also extracted. The mean values of these parameters were calculated, or pooled meta-analysis was performed if available. Ten articles were included in this systematic review, with a total of 116 patients and a follow-up period between 23 and 61 months. The mean preoperative Cobb angle and kyphosis angle were 60.1° and 38.0°, respectively, and improved to 35.4° and 26.1° postoperatively. At final follow-up, the Cobb and kyphosis angles were maintained at 36.9° and 36.0°, respectively. The average preoperative T1–T12 and T1–S1 lengths were 180.6 mm and 293.6 mm, respectively, and increased to 198.3 mm and 320.3 mm postoperatively. T1–T12 and T1–S1 lengths were 212.3 mm and 339.3 mm at final follow-up, respectively. The overall rate of patients with complications was 48% (95% confidence interval [CI], 0.38–0.58) and unplanned reoperation 44% (95% CI, 0.33–0.55) after sensitivity analysis. The current evidence from different countries with a minimum of a 2-year follow-up suggests that magnetically controlled growing rods are an effective technique to treat pediatric scoliosis and promote spine growth. However, nearly half of patients still developed complications or required unplanned reoperations.
Introduction
Early-onset scoliosis is defined as scoliosis diagnosed before 10 years of age [1,2] and has multiple etiologies, including neuromuscular, congenital, syndromic, and idiopathic. The progression of early-onset scoliosis results in cosmetic disfigurement, cardiopulmonary disorders, and early mortality [3]. Surgical treatment is indicated for children with progressive curves of >45° [4,5]. The aim of the surgical treatment is to stop the progression of the curve and allow for growth of the spine, lungs, and thoracic cage. Therefore, the spinal fusion technique is not recommended for patients with early-onset scoliosis (scoliosis diagnosed before 10 years of age) who still have growth potential.
The consensus standard technique is a growth-sparing technique using traditional growing rods to treat early-onset scoliosis in patients with remaining growth potential [4,6]. However, the major disadvantage of traditional growing rods is their requirement for operative distraction under general anesthesia every 6 months, meaning that the entirety of treatment may require more than 15 operations [1,7], which adds considerable cost and leads to loss of schooling for the children because of the repeated hospital admissions. Also, this technique has a high rate of complications and unplanned reoperations [2,7,8].
A novel device known as magnetically controlled growing rods was developed to treat pediatric scoliosis to avoid regular and repeated operations under general anesthesia [9,10]. This method has shown satisfactory preliminary clinical outcomes [11-14], and the use of ultrasound to monitor the distraction avoids radiation exposure [15,16]. However, most studies in the literature have minimum follow-up periods of less than 2 years [17-22]. Additionally, the number of cases reported in the most recent literature is less than 30, with most studies reporting less than 10 cases. Moreover, with the widespread use of magnetically controlled growing rods, the phenomenon of ‘the law of diminishing returns,’ rod slippage, metallosis, complications, and unplanned reoperations have been reported [23-28]. Therefore, we conducted the present study to systematically review the data on magnetically controlled growing rods for the treatment of early-onset scoliosis with a minimum of 2-year follow-up.
Methods and Materials
This is a systematic review of previous reports and does not require institutional ethical approval. Our present systematic review was performed in accordance with preferred reporting items for systematic review and meta-analysis (PRISMA) guidelines [29,30] (Supplemental Table 1).
1. Inclusion and exclusion criteria
Inclusion criteria were as follows: (1) patients with early-onset scoliosis diagnosed before 10 years of age, (2) patients who underwent implantation of magnetically controlled growing rods (both primary and conversion cases), and (3) minimum of 2-year follow-up. Exclusion criteria were as follows: (1) studies from the same sites with the same data extracted and (2) review articles.
2. Search strategy and study selection
Two authors (A.M.W. and J.L.L.) independently searched the electronic literature database of Medline and Embase for studies relevant to the use of magnetically controlled growing rods in the treatment of early-onset scoliosis from the first report in May 2012 to January 2018. The following keywords were searched: ‘magnetically controlled growing rod,’ ‘magnetic controlled growing rod,’ ‘magnetic growing rod,’ or ‘magnetically growing rod.’ The ‘related articles’ function was also used in the search to access additional references. Also, references from previous systematic reviews were manually searched to avoid initially overlooked publications. After the two authors independently assessed the potential eligible studies, any disagreements were discussed and resolved by a third independent author (K.Y.H.K). An updated search was performed on June 21, 2018, to include the most recent studies.
3. Data collection
The characteristics and results of the included studies were extracted by two independent reviewers (A.M.W., H.M.J.). The following information was included: author, year of publication, region/country, number of cases, age, sex, study design, follow-up duration, distraction frequency, number of distractions, distracted length, Cobb angle, kyphosis, T1–T12 length, T1–S1 length, number of complications, and frequency of unplanned reoperations.
4. Risk of bias assessment
The risk of bias of the included studies was assessed by the Joanna Briggs Institute (JBI) critical appraisal checklist for case series [31], which has a total of nine items (Supplemental Table 2). The judgments of reviewers were classified as ‘yes,’ ‘no,’ ‘unclear,’ or ‘not available.’
5. Statistical analysis
Data regarding Cobb angle, kyphosis angle, T1–T12 length, T1–S1 length at preoperative, postoperative, and final follow-up were extracted from every included study. Data on primary and revision cases were extracted separately if data in the originally included studies were reported separately. The mean values of the above parameters were calculated and presented as a line chart to depict changes at different follow-up time points. The pooled analysis of complications and unplanned reoperations was performed on STATA software ver. 12.0 (Stata Corp., College Station, TX, USA). A fixed-effects model was used to combine the data from individual studies. Heterogeneity was assessed using the I2 and χ2. If the p-value of χ2 test was <0.10 or I2 >50%, a sensitivity analysis was conducted by removing a study and evaluating whether the other results would be markedly affected.
Results
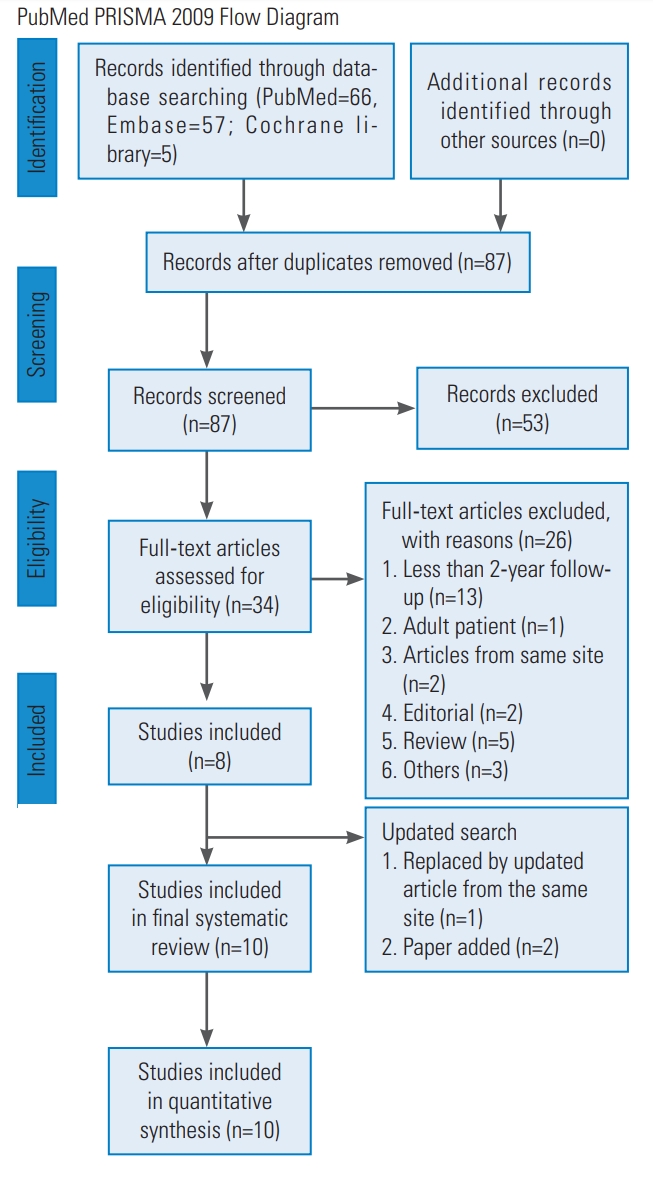
A total of 128 potential studies were identified through PubMed (n=66), Embase (n=57), and the Cochrane library (n=5). After excluding 41 duplicate articles, the remaining 87 articles were screened by title and abstract, which eliminated 53 unrelated articles or conference abstracts. In total, 34 articles were analyzed for full-text review. The studies of Cheung et al. [15] and Akbarnia et al. [32] were not included in the present systematic review because two other studies from the same sites (but with more cases) were already included in the analysis [25,33]. Eight articles from seven medical sites were included first [13,14,25,33-37]. An updated search yielded two new articles [38,39], and the article from Cheung et al. [13] was replaced by their new updated article [24] which included more cases. Although the cases from Cheung et al. [24] and Kwan et al. [25] were from the same site, only data of the Cobb angle, complications, and unplanned reoperations were reported in the study by Kwan et al. [25]; therefore, the study by Cheung et al. [24] was also included to analyze kyphosis data, T1–T12 length, and T1–S1 length. Finally, 10 articles were included in the present systemic review and quantitative analysis. The PRISMA flow diagram of article selection is shown in Fig. 1.
1. Characteristics of included studies
The first article regarding magnetically controlled growing rods for treatment of early-onset scoliosis was published in Lancet in 2012 [13] and contained only two cases with a follow-up duration of 2 years. Ten publications included a total of 116 patients (50 males and 66 females) [14,24,25,33-39]. The cases from articles by Cheung et al. [24] and Kwan et al. [25] were counted only once. All studies had a minimum follow-up period of 2 years (range, 24–61 months), except for one case in Hickey et al. [14] with a 23-month follow-up; this was also included in the present systematic review after discussion among the authors. The detailed characteristics of all included studies are shown in Table 1. The JBI critical appraisal outcomes are summarized in Supplement Table 2 in the supplement.
2. Cobb angle and kyphosis
Nine studies reported the Cobb angle preoperatively, postoperatively, and at the final follow-up [14,24,25,33-35,37-39]. However, since the articles by Cheung et al. [24] and Kwan et al. [25] were from the same site, we only used the Cobb angle data from Kwan et al. [25] for quantitative synthesis, yielding a total of 108 cases. The average Cobb angle was 60.1° preoperatively and improved to 35.4° postoperatively; the Cobb angle was maintained at 36.9° at the final follow-up. The average Cobb angles of the primary and revision subgroups were 65.9° and 47.2° preoperatively, changed to 35.2° and 42.9° postoperatively, and maintained at 36.9° and 43.8° at the final follow-up, respectively (Fig. 2).

Average Cobb angle was 60.1° preoperatively, changed to 35.4° postoperatively, and was maintained at 36.9° at final follow-up. The average Cobb angles of primary and revision subgroup were 65.9° and 47.2° preoperatively, changed to 35.2° and 42.9° postoperatively, and maintained at 36.9° and 43.8° at the final follow-up, respectively.
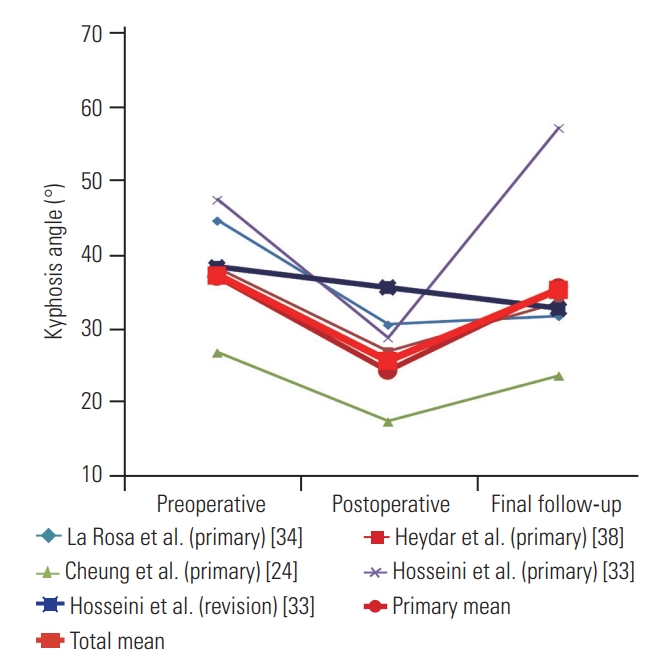
Four studies reported a kyphotic angle for a total of 68 cases [24,33,34,38]. The average kyphotic angle was 38.0° preoperatively and changed to 26.1° postoperatively; a kyphotic angle of 36.0° was observed at the final follow-up. The average kyphotic angle in the primary subgroup was 37.8° preoperatively, changed to 24.7° postoperatively, and was 36.3° at the final follow-up (Fig. 3).
3. T1–T12 and T1–S1 length
Five studies reported T1–T12 length data, for a total of 78 cases [24,33,34,38,39]. The average preoperative T1–T12 length was 180.6 mm, which increased to 198.3 mm postoperatively. At the final follow-up, T1–T12 length was 212.3 mm. The primary subgroup data could be combined, yielding mean values of 181.7 mm preoperatively, which changed to 199.7 mm postoperatively and was 216.0 mm at the final follow-up (Fig. 4).
Six studies reported T1–S1 length data, for a total of 86 cases [14,24,33,34,38,39]. The average preoperative T1–S1 length was 293.6 mm, which increased to 320.3 mm postoperatively. At the final follow-up, T1–S1 length was 339.3 mm. The average T1–S1 lengths of the primary and revision subgroups were 295.5 mm and 282.0 mm preoperatively, increased to 322.6 mm and 305.8 mm postoperatively, and were 344.5 mm and 306.9 mm at the final follow-up, respectively (Fig. 5). All the extracted data are summarized in Table 2.

The average preoperative T1–S1 length was 293.6 mm and increased to 320.3 mm postoperatively. At the final follow-up, it was 339.3 mm. The average T1–S1 length of primary and revision subgroup was 295.5 mm and 282.0 mm preoperatively and increased to 322.6 mm and 305.8 mm postoperatively; at the final follow-up, these lengths were 344.5 mm and 306.9 mm, respectively.
4. Distraction frequency and distracted length
Data of distraction frequency, number of distractions, and distracted length are summarized in Table 2. The distraction frequency was 1–2 months reported in studies by Cheung et al. [24], Hickey et al. [14], and Teoh et al. [35]. The distraction frequency was 3–6 months in studies conducted by La Rosa et al. [34], Yilmaz et al. [36], Nnadi et al. [39], and Yoon et al. [37]. The average postoperative distracted length was 28.3 mm (range of follow-up, 23–61 months) in the present systematic review. The average Cobb angle, kyphosis angle, T1–T12 length, and T1–S1 length in the cases with the higher distraction frequency (1–2 months) were 2.6°, 6.4°, 24.1 mm, and 25.3 mm, respectively, which was slightly better than patients with lower distraction frequency (3–6 months) of 3.0°, 1.2°, 12.5 mm, and 27.3 mm, respectively.
5. Complications and unplanned reoperations
Eight studies [14,25,33-35,38,39] reported complications, and seven studies [14,25,33-35,39] reported unplanned reoperations. Reasons for complications included rod breakage, failure of proximal foundation, failure of rod distraction, hook prominence, hook or screw pullout, proximal failure, proximal kyphosis, and infection. The complications and unplanned reoperations from the reported studies are summarized in Table 3.
The overall complication rate was 31% (95% confidence interval [CI], 0.23–0.39), although there was significant heterogeneity (I2=71.4%, p<0.001). Therefore, we performed a sensitivity analysis and found that the category ‘Heydar et al. (primary) [38]’ was the source of the significant heterogeneity (Supplemental Fig. 1). The overall rate of patients with complications (after omission of the category ‘Heydar et al. (primary) [38]’) was 48% (95% CI, 0.38–0.58) with no significant heterogeneity observed (I2=0.0%, p=0.685). The rate of complications for the primary and revision subgroups was 43% (95% CI, 0.31–0.56) and 48% (95% CI, 0.30–0.67), respectively (Fig. 6).
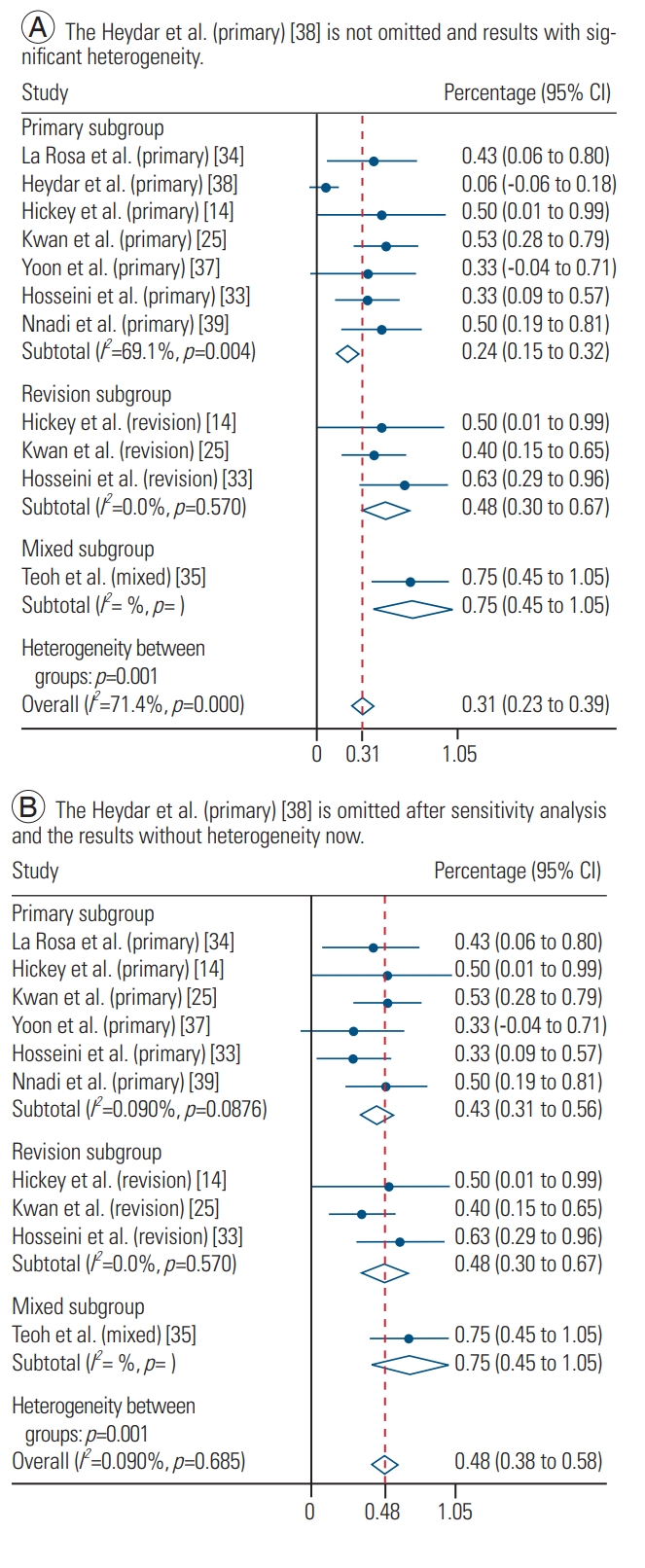
(A, B) The forest plot showed the overall rate of patients with complications of 31% (95% CI, 0.23–0.39) but with significant heterogeneity (I2=71.4%, p<0.001). After sensitivity analysis and the omission of the category ‘Heydar et al. (primary) [38],’ the overall rate of patients with complications was 48% (95% CI, 0.38–0.58), with no significant heterogeneity observed (I2=0.0%, p=0.685), primary and revision subgroup rate of 43% (95% CI, 0.31–0.56) and 48% (95% CI, 0.30–0.67), respectively. CI, confidence interval.
A pooled analysis determined that the overall rate of patients with unplanned reoperation was 75% (95% CI, 0.68–0.82) with significant heterogeneity (I2=85.6%, p<0.001). A sensitivity analysis found the category ‘Teoh et al. (primary) [35]’ was the source of the significant heterogeneity (Supplemental Fig. 2). The overall unplanned reoperation rate after omission of the category ‘Teoh et al. (primary) [35]’ was 46% (95% CI, 0.33–0.57), with no significant heterogeneity observed (I2=0.0%, p=0.795). The rate of unplanned reoperations in the primary and revision subgroups was 45% (95% CI, 0.32–0.58) and 48% (95% CI, 0.30–0.67), respectively (Fig. 7).
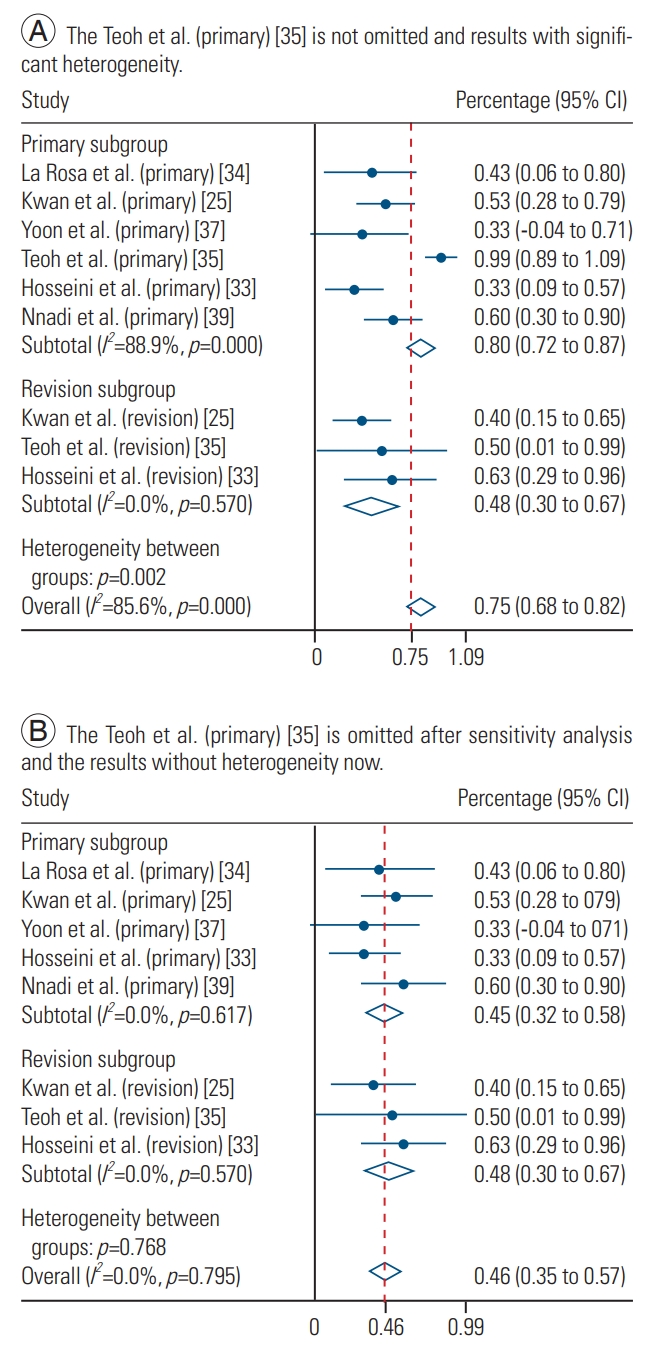
(A, B) The forest plot shows pooled analysis found that the overall rate of patients with unplanned reoperation was 75% (95% CI, 0.68–0.82), but with significant heterogeneity (I2=85.6%, p<0.001). After sensitivity analysis, the omission of the category ‘Teoh et al. (primary) [35]’ and then the overall rate of patients was 46% (95% CI, 0.33–0.57). No significant heterogeneity was observed (I2=0.0%, p=0.795). The primary and revision subgroup rate of patients with unplanned reoperation was 45% (95% CI, 0.32–0.58) and 48% (95% CI, 0.30–0.67), respectively. CI, confidence interval.
Discussion
Since Cheung et al. [13] first reported on five cases of scoliosis treated with magnetically controlled growing rods in 2012 (of only two had a 2-year follow-up), magnetically controlled growing rods have become popularized worldwide [40,41]. However, most of the published literature present only preliminary results with a short-term follow-up period of less than 2 years, and thus results with at least a 2-year follow-up are still limited. Moreover, due to the relatively low incidence of severe early-onset scoliosis, the sample size in each published study is small, with the largest study by Kwan et al. [25] which included 30 cases. We systematically reviewed ten studies [14,24,25,33-39] with a total number of 116 cases.
The Cobb angle was significantly corrected after the initial operation in patients in the primary subgroup (from 65.9° preoperative to 35.2° postoperative). However, we found that for patients for whom the magnetically controlled growing rods were used as a revision, there was only a small change in the Cobb angle (from 47.2° preoperative to 42.9° postoperative). The original data showed an average change of 3° in four revision cases in the study by Teoh et al. [35] and a 5.6° change in eight revision cases as reported by Hosseini et al. [33]. At the final follow-up, the improvements in Cobb angle were maintained. This result is mostly expected since in revision cases, most of the curves have already been corrected by the index operation, and thus, the exchange of the implant to magnetic growing rods facilitates noninvasive outpatient distractions. We also found the Cobb angle was mostly corrected during the first operation, and although further frequent distractions increased the length, the average Cobb angle did not change significantly.
The average T1–T12 and T1–S1 lengths increased to17.7 mm and 26.7 mm after the initial operation, respectively. The magnetically controlled growing rods permit increases in T1–T12 and T1–S1 length after distractions, with an average of 16.3 mm and 19.0 mm at a follow-up of more than 2 years (range, 23–61 months), respectively. However, in a study by Hosseini et al. [33] in eight patients where magnetically controlled growing rods were used as a revision, the T1–T12 and T1–S1 lengths decreased from 185.7 mm and 294.4 mm postoperatively to 180.2 mm and 290.2 mm, respectively, at the final follow-up. The average postoperation T1–S1 length in the revision subgroup was 305.8 mm and 306.9 mm at the final follow-up, a marginal 1.1 mm increase. A separate analysis found that the primary subgroup had a larger increase in T1–T12 and T1–S1 lengths with an average of 16.3 mm and 21.9 mm, respectively. In the study by Cheung et al. [13], the patients had an average of 29 mm increase in T1–S1 length 2 years after the operation, and similarly, La Rosa et al. [34] reported an average increase in the T1–S1 length of 24.2 mm after 31±5.1 months (range, 26–41 months) of follow-up. Also, Hickey et al. [14] (primary subgroup) reported one patient who had proximal junctional kyphosis and a T1–S1 length of 256 mm which was decreased to 235 mm at the final follow-up; therefore, this data point likely diluted any average increase in length in their study.
Bess et al. [7] reviewed 140 patients with early-onset scoliosis who were treated with traditional growing rods and observed a total of 177 complications, with an average of 1.2 (range, 0–7) complications per patient. Our subgroup analysis found the primary (42%) and revision (48%) subgroups had similar rates of complications. When all of the subgroups (primary, revision, and mixed) were combined, the overall rate of patients with complications was 48% (95% CI, 0.38–0.58), which is less than that of patients treated with traditional growing rods.
The overall unplanned reoperation rate after sensitivity analysis was approximately 46% (95% CI, 0.35–0.57), which meant that almost half of patients had unplanned reoperations at more than 2 years (range, 23–61 months) of follow-up. However, traditional growing rods require at least 3–4 reoperations for distraction at 2 years. In the study conducted by Bess et al. [7], 140 patients underwent a total of 897 traditional growing rod surgical procedures; on an average, each patient underwent 6.4 procedures. Therefore, magnetically controlled growing rods offer a significant advantage of decreasing the rate of multiple reoperations, thus allowing for noninvasive distraction and reducing infection rate [1,42,43].
Magnetically controlled growing rods have only been used in clinical practice for less than ten years since its first implantation in patients. There are several unresolved issues that require further investigation, such as the ‘law of diminishing returns’ after serial distraction [44], metal ion (titanium and possibly aluminum) release into serum [45], and long-term effects of tissue metallosis [27].
There are some limitations to the present systematic review that warrant discussion. First, all included studies were case series, and none were randomized controlled trials [46]. Therefore, the current evidence is still of relative low quality. Second, the sample size was still small, although our study represents the largest number of patients with a minimum of 2-year follow-up in the literature. Third, some identical cases may inadvertently been included in different studies, even though authors attempted to exclude known identical cases from the same clinical site. Fourth, data from some of the included studies only provided the mean but not the standard deviation; therefore, we could only calculate the mean values of Cobb angle, kyphosis, T1–T12, and T1–S1 length. Fifth, studies from different medical sites had different distraction frequencies and methodologies, which may thus contribute to the heterogeneity. To address this, we performed a sensitivity analysis to diminish this effect. Due to the apparent and now obvious advantages of magnetically controlled growing rods, it would be scientifically and medically unethical to conduct a randomized controlled study. Therefore, our present study provides the best evidence regarding clinical outcomes and reduced complications of magnetically controlled growing rods for the treatment of pediatric scoliosis at this time.
Conclusions
The present systematic review of studies who observed more than 2-year follow-up suggests that the use of magnetically controlled growing rods is an effective technique in the treatment of pediatric scoliosis as it permits spinal growth and is associated with fewer complications and unplanned reoperations compared to traditional growing rods. However, surgeons still must note the significant risk of complications and unplanned reoperations. Further studies should be conducted across multiple centers and include a full long-term follow-up of patients from implantation of magnetically controlled growing rods to final fusion.
Notes
K.M.C.C. received grant and research support from Ellipse Technologies (now belonged to Nuvasive) and is consultants for the company. No potential conflict of interest relevant to this article was reported.
Supplementary Materials
Supplementary materials can be found via https://doi.org/10.31616/asj.2018.0272.
PRISMA 2009 checklist.
Joanna Briggs Institute critical appraisal checklist for case series of included studies.
Sensitivity analysis indicating that the category of Heydar et al. (primary) [38] significantly contributed to the heterogeneity of complication rate.
Sensitivity analysis indicating that the category of Teoh et al. (primary) [35] significantly contributed to the heterogeneity of rate of unplanned reoperations.