|
 |
- Search
| Asian Spine J > Volume 12(2); 2018 > Article |
|
Abstract
Purpose
This study aimed to evaluate the efficacy of minimally invasive transtubular endoscopic decompression for the treatment of lumbosacral extraforaminal lesion (LSEFL).
Overview of Literature
Conventional procedures for surgical decompression for the treatment of LSEFL involve certain technical challenges because the lumbosacral extraforaminal region has unique anatomical features. Moreover, the efficacy of minimally invasive procedures performed via the posterolateral approach for LSEFL has been reported.
Methods
Twenty-five patients who had undergone minimally invasive transtubular endoscopic decompression for the treatment of LSEFL and could be followed up for at least 1 year postoperatively were enrolled. Five of these patients had a history of lumbar surgery, and seven had concomitant adjacent-level spinal stenosis. The clinical outcomes were evaluated using the Japanese Orthopaedic Association (JOA) lumbar score, numeric rating scale (NRS), and the JOA Back Pain Evaluation Questionnaire (JOABPEQ). The mean postoperative follow-up (FU) duration was 3.8 years.
Results
All procedures could be completed without any severe surgical complications, and all patients could resume their previous activity level within 1 month postoperatively. The JOA score significantly increased from 14.1±4.0 at baseline to 23.1±3.7 at the 1-year FU and 22.1±3.8 at the last FU. Similarly, there were significant improvements in the postoperative NRS and JOABPEQ scores. An additional surgery was performed in two patients (8%) during the FU period. Patients with degenerative scoliosis exhibited significantly poorer outcomes compared with those without this condition.
Conclusions
Transtubular endoscopic decompression can overcome certain technical challenges involved in the conventional procedures for LSEFL treatment; therefore, it can be recommended as a useful procedure for treating LSEFL. This procedure can provide some benefits to LSEFL patients and offer a well-illuminated surgical field and high surgical safety for the surgeon. However, the procedure should be carefully adapted for LSEFL patients with concomitant degenerative scoliosis.
L5 radiculopathy is commonly caused by L4–L5 lesions. However, foraminal and extraforaminal lesions at L5–S1 can also occasionally induce L5 radiculopathy. Extraforaminal disc herniation at L5–S1 accounts for approximately 2%–4% of all symptomatic lumbar disc herniations. [12] In contrast, several researchers have reported that extraforaminal lumbar nerve compression by bony or ligamentous structures can cause L5 radiculopathy from the first description by Wiltse et al. [3], and it has been recently hypothesized that the incidence of these lesions might have been underestimated, particularly in the elderly [245]. Nevertheless, lumbosacral extraforaminal lesions (LSEFLs) are considerably more uncommon than intraspinal canal lesions at L4–L5 as the cause of L5 radiculopathy. Consequently, LSEFLs are often misdiagnosed and overlooked, resulting in the failed back surgery syndrome [5].
Surgical intervention should be considered for LSEFL patients who do not respond to conservative treatments. The surgical intervention for LSEFL includes total facetectomy and fusion as well as decompression alone using the midline approach or the posterolateral approach. Previously, the common surgical procedure used was total facetectomy with or without fusion via the midline approach. This was followed by decompression alone using the midline or posterolateral approaches such as the inter- or intramuscular route [67]. However, surgical access to the L5–S1 extraforaminal region is complicated, unlike that to the upper lumbar segments [8]. The lumbosacral extraforaminal region is further laterally and deeply placed, making it challenging to access it via the midline approach. Moreover, the prominent iliac crest might narrow the surgical corridor through a posterolateral muscle-splitting posterolateral approach. Minimum access techniques that involve the use of a tubular retractor overcome these limitations and enable easy access to the region; however, they limit the extent of exposure. We performed tubular surgery with the assistance of endoscopic techniques to treat LSEFL [910111213]. The present study aimed to evaluate the clinical outcomes of minimally invasive transtubular endoscopic decompression for LSEFL.
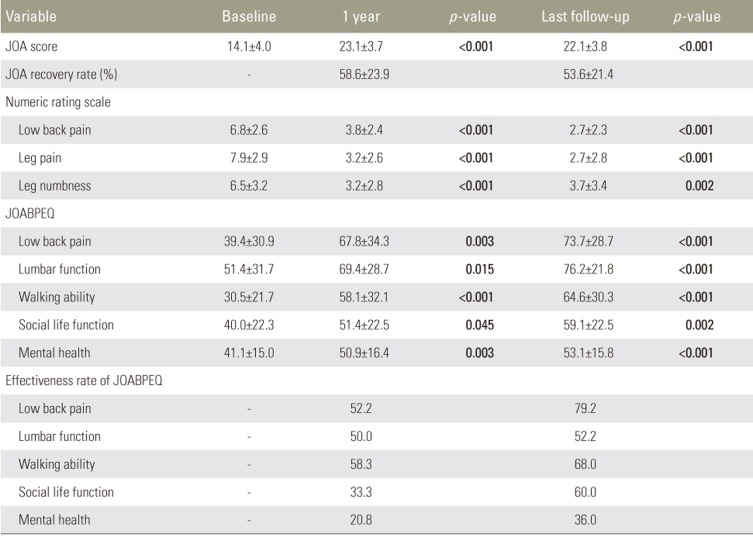
Between June 2008 and February 2016, 30 LSEFL patients who did not respond to conservative treatments were surgically treated using minimally invasive transtubular endoscopic decompression in Karatsu Red Cross Hospital. Four patients were lost to follow-up (FU), and one died of a heart attack at 3 years postoperatively. The remaining 25 patients who could be followed up for at least 1 year postoperatively were enrolled. The FU rate was 83.3%. The study population comprised seven men and 18 women with a mean age at the time of surgery of 67.4 years (range, 37 to 84 years). Extraforaminal disc herniation was observed in 13 patients. Concomitant adjacent-level spinal stenosis (L4–L5) was observed in seven patients, including four patients with L4 degenerative spondylolisthesis. Five patients were found to have a history of lumbar surgery; two of these patients only experienced slight relief following their previous surgery, while the remaining 3 reported substantial improvement postoperatively. In these patients, the mean duration between the previous surgery and the index surgery was 3.8 years (range, 0.25 to 9 years). Patients' demographic data are summarized in Table 1.
All patients complained of low back pain (LBP) and leg symptoms, and the mean preoperative symptom duration was 16 months. During the objective evaluations, leg sensory disturbance was observed in 20 patients; decreased leg muscles strength, particularly in the toe extensors, was noted in 24 patients. Three patients experienced mild causalgia (complex regional pain syndrome type II [CRPS type II]).
LSEFL was diagnosed based on clinical symptoms, neurological findings, and diagnostic imaging findings. Temporary pain relief following selective L5 nerve block and the findings of L5 radiculography were very helpful in establishing a diagnosis of LSEFL. In addition, seven patients with adjacent-level severe spinal stenosis that was significant enough to warrant decompression underwent concomitant transtubular endoscopic decompression at L4–L5 [1415]. The postoperative FU duration ranged from 12 to 81 months (mean, 46 months).
Preoperatively, the surgeon should ideally evaluate whether the tubular retractor can reach the extraforaminal region at the lumbosacral junction via the posterolateral approach without any obstruction of the prominent iliac crest using axial computed tomography (CT) images. However, in few cases, the prominent iliac crest hinders the passage of the tubular retractor to the extraforaminal region.
The surgical procedure was performed with the patient in the prone position and under general analgesia. The METRx MED system (Medtronic Sofamor Danek, Memphis, TN, USA) was used for the entire procedure. A vertical 2-cm skin incision was marked approximately 1 cm lateral to the lateral margin of the L5–S1 facet joint, using an image intensifier. The incision was deepened to the level of the lumbar fascia. Serial dilators were passed to gently dilate the lumbar paraspinal muscles and to retract the lumbodorsal fascia. Thereafter, a 16-mm tubular retractor was passed over the dilators and was secured to a flexiblearm retractor mounted on the side rail of the table. The dilators were then removed, and the endoscope (25° angle) was attached to the tubular retractor (Fig. 1A, B).
A high-speed drill was used to perform drilling that was started at the base of the lateral aspect of the superior articular process (SAP) of S1 and continued superiorly and laterally for partial resection of the S1 SAP and the sacral ala. The next step involved the partial removal of the inferior aspect of the L5 transverse process. After the bony resection was complete, the lumbosacral ligaments were detached from the sacral ala and the L5 transverse process (Fig. 1C). Following the resection of the lumbosacral ligaments, the L5 spinal nerve is usually identified at the extraforaminal zone by performing dissection of the overlying fat tissue and the blood vessels (Fig. 1D). We performed an aggressive discectomy for all the patients (Fig. 1E). However, no attempt was made to remove the osteophytes of the vertebral bodies to prevent further nerve damage. In cases where we observed osteophyte formation owing to a pseudoarticulation between the L5 transverse process and the sacral ala, we resected the osteophyte. In patients with concomitant foraminal stenosis, partial resection of the cranial tip of the S1 SAP was performed. Decompression was considered complete when the L5 spinal nerve was released from the foraminal portion to the depth of the lumbosacral tunnel at which point it entered the pelvic cavity (Fig. 1F).
After inspecting the L5 nerve root, the site was copiously irrigated using physiological saline. The tubular retractor and endoscope were withdrawn. Thereafter, a suction drain was placed in the dorsal space of the L5 spinal nerve to prevent postoperative hematoma, and the fascia and the skin were closed routinely.
All the patients were encouraged to stand up and walk on postoperative day 1. The patients were discharged from the hospital at 1 week postoperatively and were able to resume their previous activities within 1 month postoperatively.
Clinical assessments were conducted using the Japanese Orthopaedic Association (JOA) lumbar score (range, −6 to 29 points) and its recovery rate; JOA Back Pain Evaluation Questionnaire (JOABPEQ) score; and numeric rating scale (NRS) score for LBP, leg pain, and leg numbness preoperatively, 1 year postoperatively, and at the last FU.
The JOA recovery rate was calculated according to the Hirabayashi method. The formula to calculate the recovery rate was as follows: {postoperative JOA score-preoperative JOA score/(29-preoperative JOA score)}×100 (%).
The JOABPEQ is an outcome measure used for evaluating LBP; it includes several aspects and is based on patient subjectivity. The score includes the following five domains: LBP, lumbar function, walking ability, social life function, and mental health. The score for each domain ranges from 0 to 100, with higher scores indicating a better condition. The data of JOABPEQ were processed as per the directions for use described by Fukui et al. [16].
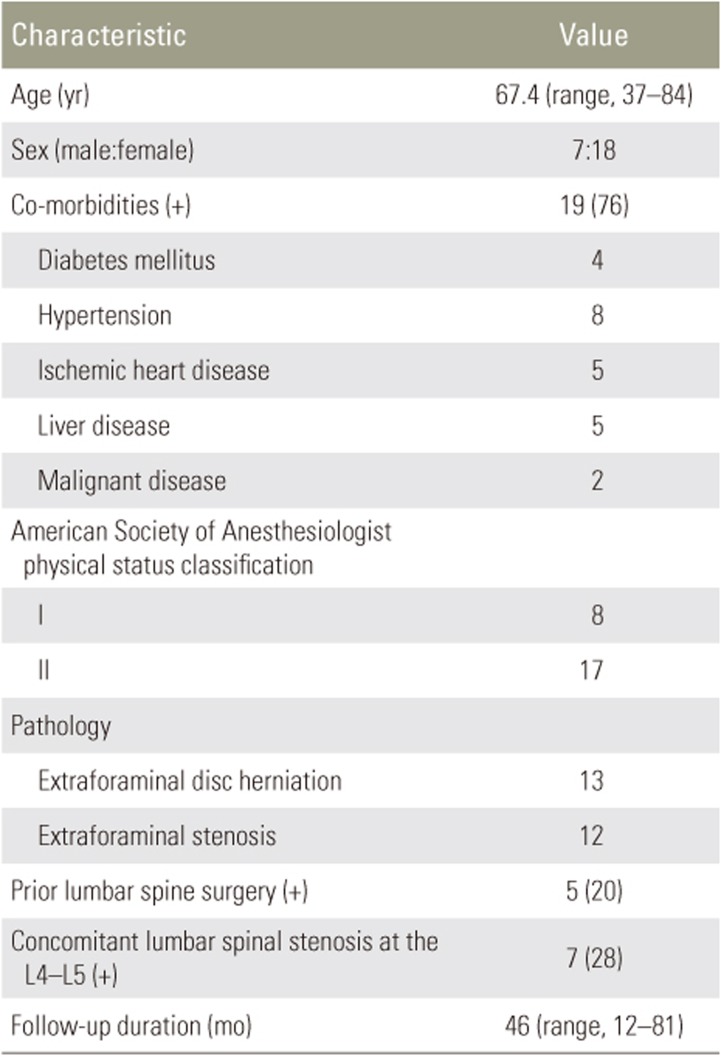
Pre- and postoperative imaging studies, including plain radiography, CT examination, and magnetic resonance imaging, were conducted. The presence or absence of degenerative lumbar scoliosis, the curve and magnitude of the Cobb's angle, and the laterality and degree of coronal wedging at L5–S1 were evaluated using the plain radiographs. The degree of coronal wedging at L5–S1 was noted as the angle between the lines drawn through the superior endplates of L5 and S1 (Fig. 2A). When the superior endplate of S1 was unclear, a line joining the superior points on the sacral ala was used as a reference (Fig. 2B). The grade of extraforaminal stenosis caused by the bony structures, such as the osteophyte formation of the L5 and S1 vertebral body and forming a pseudoarticulation with the sacrum, was assessed using axial, coronal, and reconstructed three-dimentional CT scans. The preservation of the facet joints after the surgical procedure was evaluated using postoperative CT scans. The grade of disc degeneration was assessed using the Pfirrmann classification on sagittal T2-weighted magnetic resonance images [17].
Descriptive data are presented as mean and standard deviation values or frequencies (%). The significances of differences were statistically analyzed using unpaired t-test, paired t-test, and the Mann-Whitney U-test. All p-values <0.05 were considered statistically significant.
The mean surgical duration was 93 minutes (range, 56 to 138 minutes), and the mean estimated blood loss (EBL) during the procedure was 8.1 mL (range, uncountable to 75 mL). The EBL was uncountable in 19 patients (76%). Accidental root sleeve injury and root injury were not observed in any patient. A fracture of the L5 transverse process was noted on the postoperative CT scans in four patients (16%); however, the fracture was asymptomatic with no effect on postoperative recovery. All the patients could stand up and walk on postoperative day 1. No patient experienced surgical-site infection or neurological deterioration. Three patients who experienced mild CRPS type II preoperatively demonstrated no symptom deterioration after the surgery. The mean hospital stay duration was 10 days (range, 8 to 19 days), and all patients were able to resume their previous activities within 1 month postoperatively.
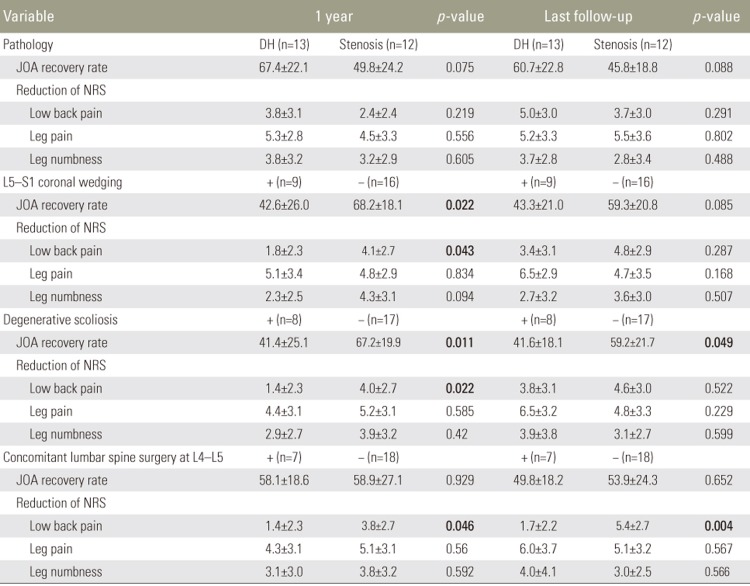
The JOA score significantly increased from 14.1±4 at baseline to 23.1±3.7 at the 1-year FU (p<0.001) and to 22.1±3.8 at the last FU (p<0.001). The JOA recovery rates were 58.6%±23.9% at the 1-year FU and 53.6%±21.4% at the last FU. The preoperative NRS scores for LBP, leg pain, and leg numbness were 6.8±2.5, 7.9±2.8, and 6.5±3.2, respectively. Further, the NRS scores for LBP, leg pain, and leg numbness at the 1-year FU and the last FU decreased significantly to 3.8±2.4 and 2.7±2.3, 3.2±2.6 and 2.7±2.8, and 3.2±2.8 and 3.7±3.4, respectively. The JOABPEQ analysis revealed that the mean functional scores for all domains had improved significantly at the 1-year FU and the last FU. With respect to LBP, lumbar function, and walking ability, the effectiveness rates of JOABPEQ were >50% at the 1-year FU and the last FU. Although the effectiveness rate on the domain social life function was 33.3% at the 1-year FU, it increased to 60% at the last FU. The clinical outcomes have been summarized in Table 2. Two patients underwent revision surgery during the FU duration. The reasons for revision surgery included a recurred foraminal disc herniation of L5–S1 at 3.3 years postoperatively (after the index surgery) and a foraminal stenosis of L3–L4 due to concomitant degenerative scoliosis at 7 months after the index surgery. Both patients reported symptom relief following the revision surgery.
On preoperative imaging, purely extraforaminal disc herniation was demonstrated in 13 patients, whereas concomitant adjacent-level spinal stenosis (L4–L5) was noted in seven. Concomitant foraminal stenosis was strongly suspected in three patients. Degenerative scoliosis (Cobb angle ≥10°) was observed in eight patients, and coronal wedging at L5–S1 (≥5°) was observed in nine patients. Osteophyte formation at the posterolateral edge of L5 and S1 vertebral bodies was observed in 20 patients; six small osteophytes and 14 moderate osteophytes were detected. Pseudoarticulation between the L5 transverse process and the sacrum was noted in 10 patients. As per the Pfirrmann classification, grade of disc degeneration was grade III in six patients, grade IV in 16 patients, and grade V in three patients.
Postoperative CT scans revealed a fracture of the L5 transverse process in four patients (16%; one man and three elderly women). It was suspected that the fractures resulted from sufficient resection of the inferior aspect of the L5 transverse process for obtaining adequate decompression of the L5 nerve and osteoporosis. However, all fractures healed naturally. Complete preservation of the L5–S1 facet joint was noted in 19 patients (76%), and a small amount of partial resection of the S1 SAP was observed in the remaining six patients (Fig. 3). No patient developed postoperative segmental instability at the affected segment. However, one patient exhibited progression of concomitant degenerative scoliosis.
We conducted an analysis to identify the preoperative radiological factors associated with the surgical outcomes. We evaluated the clinical outcomes using the recovery rate of the JOA score and the reduction in the NRS score postoperatively. Consequently, the presence of concomitant degenerative scoliosis was found to be a predictor of poor outcomes, particularly for LBP reduction. However, there was no significant difference in the degree of relief in leg symptoms between the patients with and without degenerative scoliosis. In addition, coronal wedging at L5–S1 (≥5°) was identified as a risk factor for poor outcomes at 1 year postoperatively. Although patients with coronal wedging tended to have poorer outcomes than those without wedging at the last FU, this difference was not statistically significant. The type of pathology and presence of concomitant L4–L5 lesion were not identified as predictors of poor outcomes on the JOA recovery rates. However, the postoperative reduction in LBP was poor in patients with concomitant L4–L5 lesion. The results are presented in Table 3.
Surgical intervention should be considered for LSEFL patients who do not respond to conservative treatments. In recent years, only decompression via the posterolateral approaches such as the inter- or intramuscular route has gained popularity as a surgical intervention for LSEFL [6]. However, achieving surgical access to the L5–S1 extraforaminal region is complicated owing to the fact that the lumbosacral extraforaminal space has unique anatomical features and that the region is deeply located comparing with the upper lumbar segments [58]. Moreover, the prominent iliac crest may cause narrowing of the surgical corridor through the posterolateral approach. Some minimally invasive approaches to access the lumbosacral extraforaminal region have been described by various research scholars. Minimum access techniques that employ a tubular retractor help overcome these limitations and enable easy access to the region; however, these limit the extent of exposure. We performed tubular surgery with the assistance of endoscopic techniques for the treatment of LSEFL. The procedure described by Matsumoto et al. [10], O'Toole et al. [11], Yamada et al. [12], and Zhou et al. [13] was used. In the present study, we were able to successfully perform minimally invasive transtubular endoscopic decompression without severe surgical complications in all LSEFL patients. This less invasive procedure enables a well-illuminated surgical field and high surgical safety for the surgeon. The EBL was low, and the facet joint could be preserved in almost all the patients. Moreover, the procedure provided certain advantages to the patients, including mild postoperative back pain and early resumption of previous, routine activities. Consequently, transtubular endoscopic decompression appears to be a safe and useful minimally invasive procedure for the treatment of LSEFL.
Many authors have reported good clinical outcomes of performing only surgical decompression for LSEFL, including extraforaminal disc herniation and extraforaminal stenosis. Kotil et al. [1] described a minimally invasive transmuscular approach for excising the far lateral L5–S1 level herniated discs. The researchers reported satisfactory results in 92.9% of the 14 patients during a mean FU period of 29 months. Lee et al. [2] described a transtubular microscopic decompression for extraforaminal compression of the L5 nerve root at the lumbosacral junction. In this study on 52 consecutive patients who were followed up for a mean duration of 7 months, the outcomes were excellent or good in 96% patients, and the mean JOA recovery rate was 86.1% [2]. Matsumoto et al. [18] reviewed 28 patients with extraforaminal stenosis at the lumbosacral junction who had undergone posterior decompression without fusion; the researchers reported a mean JOA recovery rate of 68.5% at an average FU of 32.5 months. Yamada et al. [12] conducted a retrospective case study on 32 patients with extraforaminal stenosis at the lumbosacral junction who were treated with minimally invasive surgery using a spinal endoscope, a procedure same as that used in our study. The researchers reported a mean JOA recovery rate of 60.1% at an average FU duration of 37.4 months [12]. In our study, the mean JOA recovery rates were 58.6%±23.9% at the 1-year FU and 53.6%±21.4% at a mean FU of 46 months. Our study reported slightly lower recovery rates than previous trials. However, the mean age of the study population was higher and the mean postoperative FU duration was slightly longer in the present study than in the previous researches. Considering these factors, our results could be considered comparable with the previous reports.
Several researchers have described some preoperative predictors of poor surgical outcomes after performing only decompression for lumbar extraforaminal lesions. Chang et al. [19] conducted a trial on a series of 184 patients who had unilateral root compression lateral to the foramen caused by discs, stenosis, or both at the lumbar spine; the reports of this trial showed that the patients who required double herniation (combined intracanalicular and far lateral disc herniation at the same level) were approximately three times as likely to experience residual or recurrent postoperative leg pain than those who required lateral fenestration only. Lee et al. [20] also determined that concomitant foraminal LDH appeared to be related to postoperative residual leg pain following microdecompression for extraforaminal LDH at the L5–S1 level in a series of 65 patients. Choi et al. [21] reported that a large preoperative difference of disk height between the standing and supine positions was associated with poor clinical outcomes; these results reflect the findings of a retrospective investigation conducted on 93 patients who had undergone posterior decompression alone for foraminal and extraforaminal entrapment of the L5 nerve root. Moreover, many researchers have described that the presence of concomitant foraminal lesions, including disc herniation and stenosis, as well as inadequate decompression could be predictors of poor surgical outcomes of decompression alone for LSEFL. Several authors have reported certain challenges in differentiating foraminal, extraforaminal, and combined foraminal and extraforaminal lesions [181920]. Matsumoto et al. [18] reported that three patients from a series of 28 patients with LSEFL experienced recurrence within a relatively short duration following extraforaminal decompression caused by intraforaminal stenosis that was detected at the time of the revision surgery. Further, the authors stated that the L5–S1 tilting angle tended to be large in these patients who underwent revision surgery [18]. In the present study, patients with the coronal wedging at L5–S1 exhibited poorer outcomes than those without the wedging. However, the difference was not statistically significant at the last FU. Irrespective of the presence of coronal wedging at L5–S1, subjective leg symptoms had considerably reduced postoperatively, suggesting that adequate decompression of the L5 spinal nerve from the foraminal portion to the depth of the lumbosacral tunnel where it enters the pelvic cavity was completed in our series. In contrast, the presence of concomitant degenerative scoliosis was identified as a preoperative radiological predictor of the poor outcomes of transtubular endoscopic decompression for LSEFL. However, although there was substantial reduction in the postoperative subjective leg symptoms of patients with degenerative scoliosis, the relief in LBP at 1 year postoperatively was poor in these patients. This may indicate that the pathology of LSEFL patients with degenerative scoliosis is complicated, suggesting that LBP is caused by degenerative scoliosis itself. In patients with LSEFL and degenerative scoliosis, further detailed preoperative assessment should be performed, and the procedure should be undertaken carefully.
The limitation of the present study is that this was a retrospective observational study on a small sample size. Further, detailed prospective trials on a larger population are warranted for a deeper understanding of this subject.
Transtubular endoscopic decompression has the potential to overcome certain technical challenges of the conventional procedures for LSEFLs and can be a useful procedure for treating LSEFL. This less invasive procedure can not only provide some benefits to LSEFL patients but also enable a well-illuminated surgical field and high surgical safety for the surgeon. However, the procedure warrants careful application in LSEFL patients with concomitant degenerative scoliosis.
Notes
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
References
1. Kotil K, Akcetin M, Bilge T. A minimally invasive transmuscular approach to far-lateral L5-S1 level disc herniations: a prospective study. J Spinal Disord Tech 2007 20:132–138. PMID: 17414982.


2. Lee S, Kang JH, Srikantha U, Jang IT, Oh SH. Extraforaminal compression of the L-5 nerve root at the lumbosacral junction: clinical analysis, decompression technique, and outcome. J Neurosurg Spine 2014 20:371–379. PMID: 24460578.


3. Wiltse LL, Guyer RD, Spencer CW, Glenn WV, Porter IS. Alar transverse process impingement of the L5 spinal nerve: the far-out syndrome. Spine (Phila Pa 1976) 1984 9:31–41. PMID: 6719255.


4. Matsumoto M, Chiba K, Nojiri K, Ishikawa M, Toyama Y, Nishikawa Y. Extraforaminal entrapment of the fifth lumbar spinal nerve by osteophytes of the lumbosacral spine: anatomic study and a report of four cases. Spine (Phila Pa 1976) 2002 27:E169–E173. PMID: 11884922.


5. Tubbs RS, Iwanaga J, Aly I, et al. Extraforaminal compression of the L5 nerve: an anatomical study with application to failed posterior decompressive procedures. J Clin Neurosci 2017 41:139–143. PMID: 28408248.


6. Epstein NE. Foraminal and far lateral lumbar disc herniations: surgical alternatives and outcome measures. Spinal Cord 2002 40:491–500. PMID: 12235530.



7. Wiltse LL, Bateman JG, Hutchinson RH, Nelson WE. The paraspinal sacrospinalis-splitting approach to the lumbar spine. J Bone Joint Surg Am 1968 50:919–926. PMID: 5676831.


8. GGioia G, Mandelli D, Capaccioni B, Randelli F, Tessari L. Surgical treatment of far lateral lumbar disc herniation: identification of compressed root and discectomy by lateral approach. Spine (Phila Pa 1976) 1999 24:1952–1957. PMID: 10515022.


9. Li Y, Lubelski D, Abdullah KG, Mroz TE, Steinmetz MP. Minimally invasive tubular resection of the anomalous transverse process in patients with Bertolotti’s syndrome: presented at the 2013 Joint Spine Section Meeting: clinical article. J Neurosurg Spine 2014 20:283–290. PMID: 24358999.


10. Matsumoto M, Chiba K, Ishii K, Watanabe K, Nakamura M, Toyama Y. Microendoscopic partial resection of the sacral ala to relieve extraforaminal entrapment of the L-5 spinal nerve at the lumbosacral tunnel: technical note. J Neurosurg Spine 2006 4:342–346. PMID: 16619684.


11. O’Toole JE, Eichholz KM, Fessler RG. Minimally invasive far lateral microendoscopic discectomy for extraforaminal disc herniation at the lumbosacral junction: cadaveric dissection and technical case report. Spine J 2007 7:414–421. PMID: 17630139.


12. Yamada H, Yoshida M, Hashizume H, et al. Efficacy of novel minimally invasive surgery using spinal microendoscope for treating extraforaminal stenosis at the lumbosacral junction. J Spinal Disord Tech 2012 25:268–276. PMID: 21811183.


13. Zhou Y, Zheng WJ, Wang J, et al. The clinical features of, and microendoscopic decompression for, extraforaminal entrapment of the L5 spinal nerve. Orthop Surg 2009 1:74–77. PMID: 22009785.



15. Ikuta K, Arima J, Tanaka T, et al. Short-term results of microendoscopic posterior decompression for lumbar spinal stenosis: technical note. J Neurosurg Spine 2005 2:624–633. PMID: 15945442.


16. Fukui M, Chiba K, Kawakami M, et al. JOA Back Pain Evaluation Questionnaire (JOABPEQ)/JOA Cervical Myelopathy Evaluation Questionnaire (JOACMEQ) he report on the development of revised versions: April 16, 2007: the Subcommittee of the Clinical Outcome Committee of the Japanese Orthopaedic Association on Low Back Pain and Cervical Myelopathy Evaluation. J Orthop Sci 2009 14:348–365. PMID: 19499305.


17. Pfirrmann CW, Metzdorf A, Zanetti M, Hodler J, Boos N. Magnetic resonance classification of lumbar intervertebral disc degeneration. Spine (Phila Pa 1976) 2001 26:1873–1878. PMID: 11568697.


18. Matsumoto M, Watanabe K, Ishii K, et al. Posterior decompression surgery for extraforaminal entrapment of the fifth lumbar spinal nerve at the lumbosacral junction. J Neurosurg Spine 2010 12:72–81. PMID: 20043768.


19. Chang SB, Lee SH, Ahn Y, Kim JM. Risk factor for unsatisfactory outcome after lumbar foraminal and far lateral microdecompression. Spine(Phila Pa 1976) 2006 31:1163–1167. PMID: 16648754.


20. Lee DY, Lee SH. Microdecompression for extraforaminal L5-s1 disc herniation; the significance of concomitant foraminal disc herniation for postoperative leg pain. J Korean Neurosurg Soc 2008 44:19–25. PMID: 19096652.



21. Choi KC, Kim JS, Lee DC, Park CK. Outcome of decompression alone for f oraminal/extraforaminal entrapment of L5 nerve root through Wiltse paraspinal approach. Clin Spine Surg 2017 30:E1220–E1226. PMID: 27977444.


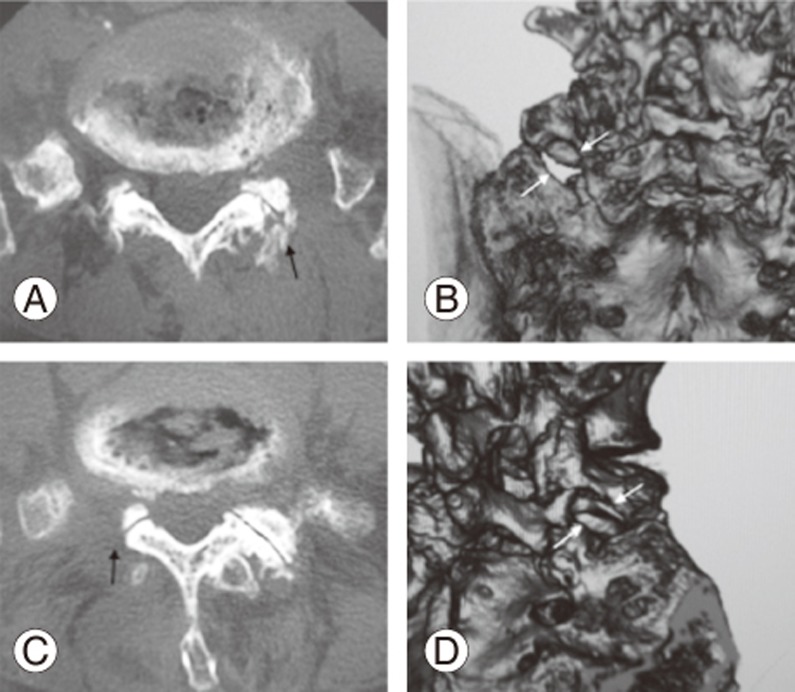
Fig. 1
Minimally invasive transtubular endoscopic decompression using METRx MED system. (A) METRx MED system (Medtronic Sofamor Danek, Memphis, TN, USA). (B) Exposing the dorsal aspect of the extraforaminal area at the lumbosacral junction on the right side. (C) The lumbosacral ligaments are detached from the sacral ala and the L5 transverse process after the completion of bony resection by the partial resection of the S1 superior articular process and the sacral ala (arrows). (D) The L5 spinal nerve is identified at the extraforaminal zone by dissecting the overlying fat tissue and blood vessels after the resection of the lumbosacral ligaments (arrows). (E) An aggressive discectomy is performed. (F) Decompression is completed when the L5 spinal nerve is released from the foraminal portion to the depth of the lumbosacral tunnel where it enters the pelvic cavity.
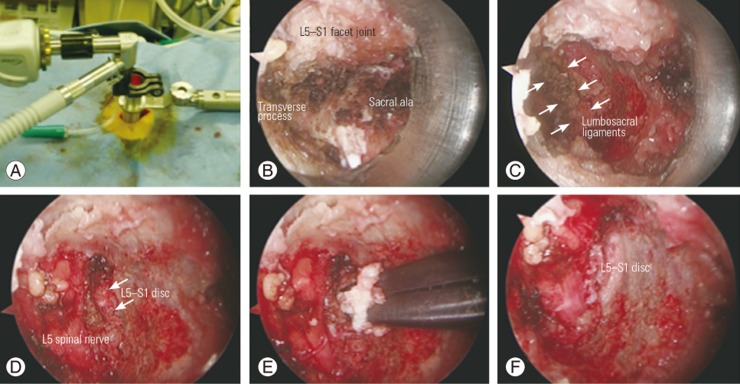
Fig. 2
Measurement of the degree of coronal wedging at L5–S1. (A) The degree of coronal wedging at L5–S1 was noted as the angle between the lines drawn through the superior endplates of L5 and S1 (★). (B) When the superior endplate of S1 was unclear, a line joining the superior points on the sacral ala was used as a reference (☆).
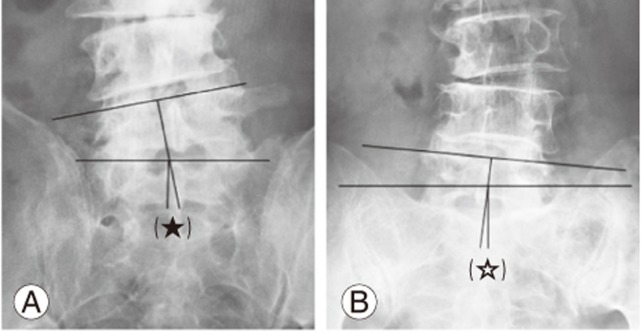
Fig. 3
Assessments of surgical invasion of the facet joint on postoperative computed tomography scans. (A, B) Complete preservation of the facet joint (black arrows). (C, D) Partial resection of the cranial tip of the S1 superior articular process (black arrows) was performed to decompress the concomitant foraminal stenosis.