Introduction
Affecting up to 2 in 3 of the adult population during the course of a year, back pain is a very common disorder [1,2]. Back pain is a leading reason for doctor consultation, hospitalisation and other health and social care service utilisation [3], and is considered as the most costly musculoskeletal disease in industrialized countries [4]. Over the last few decades, research has focused on understanding possible mechanisms responsible for low back dysfunction (LBD). The presence of spinal proprioceptive deficit in LBD population is one of the current debates that could explain the patho-physiology of back pain [5-7]. Proprioception is a special term often used to describe the complex interaction between afferent and efferent input to control body movement and position [8]. Proprioception is thought to have a key role in maintaining normal spinal movement and stability [5,9]. Many authors have demonstrated that sensory-motor deficits are present in LBD patients; these deficits can affect segmental spinal stability and eventually lead to articular damage and subsequent chronic pain [10,11]. Sensori-motor dysfunction associated with LBD may include disturbances in a wide range of control mechanisms; the patho-physiological mechanisms and characteristics of these disturbances in different spinal lesions, however, require further investigation [12].
Understanding the role of such mechanisms in normal persons and in subjects with LBD could be crucial for improving back pain management, particularly those aspects related to reaching sound diagnosis, providing plausible explanation of the problem, providing relevant information and prescribing effective rehabilitation approaches [13]; yet, research is needed to investigate such an issue [14]. Although attention was drawn to include proprioceptive re-training exercises in current back rehabilitation programs [15]; very little research, however, exists to support this [8]. Impaired proprioception may be a major risk factor for recurrent injuries after the integrity of the muscles and ligaments has been restored [16]. Proprioceptive deficits are thought to be both a consequence and a cause of injury [17]. Proprioception and muscle control training could be the main key elements for rehabilitation of patients with LBD; still, little research has attempted to quantify spinal proprioception and detect proprioceptive deficits in patients with LBD [18,19].
LBD is a frequent condition with a wide range of clinical picture and causes. Twelve years ago, it was suggested that a gap in the literature existed concerning the detection of the degree to which proprioceptive deficits occur with different spinal lesions [9]; the situation has not significantly changed and research is still needed to discern such as aspect. The purpose of this study was to determine whether repositioning accuracy as a measure of proprioception differs in subjects with and without LBD, and to investigate the difference in the degree of repositioning accuracy in relation to the cause of the LBD, whether mechanical or discogenic.
Materials and Methods
2. Subjects
The study recruited 45 participants from the local Musculoskeletal Outpatient Department. Participants were then assigned to three different groups according to their clinical presentation, signs and symptoms. Participants in group I were normal subjects with no past history of back pain that required medical care, and who were mainly attending the clinic as the relatives or carers of other patients. Participants in group II (mechanical low back dysfunction [MLBD]) had a history of non-specific, non-radicular chronic mechanical LBD, lasting more than three months, which was primarily of myogenic origin, without discogenic or arthrogenic causes. Participants in group III (discogenic low back dysfunction [DLBD]) had a clinical and radiological diagnosis of chronic LBD, lasting more than three months, and that was primarily due to a disc herniation or bulge.
3. Selection of participants
Selection of participants in the experimental groups was based on the patients' signs and symptoms, and was confirmed by the clinical and radiological investigations done by an orthopaedic surgeon. To be included in the LBD groups, participants had to report an average pain level of more than five on the Visual Analogue Scale (VAS) and a lumbar spine range of motion (ROM) of at least 50% of the accepted normal range, in order to be able to achieve the target position adopted by the study. All subjects were screened for the following exclusion criteria prior to participation; previous inner ear infection or vestibular disorder with unresolved balance disturbance, history of head trauma with residual neurological deficits, metabolic diseases such as diabetes, pregnant or lactating women, spinal surgery and severe back pain [18,20].
4. Measurement protocol
On the examination day, participants were not allowed to take any muscle relaxants or antispastic medication that may interfere with the test [20]. Participants completed consent forms that informed them of the study purpose and the procedure. The experimental groups were asked to report their pain level by using a VAS with responses ranging from "No pain" to "The worst pain." An Oswestry Disability Index (ODI), which consisted of 10 questions asking about different aspects of the back pain and its impact on function, was administered to each participant in the experimental groups, for assessment of the functional level and the induced disability [8,21]. Subjects were given verbal explanation about the purpose and procedure of the study.
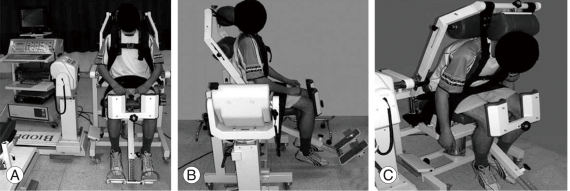
Biodex System 3 Pro Isokinetic Dynamometer (Biodex Medical Inc., Shirley, New York, NY, USA), equipped with a special forward reclined back attachment, was used for measuring the lumbar repositioning accuracy in this study. System calibration was done prior to each testing session. The participant was seated on the chair of the Biodex system, knee block positions were individually adjusted by two curved anterior leg pads, the feet were held in a position with no contact with the floor, both thighs were stabilized by two straps, the pelvic brace was then applied and positioned as far down as possible to press firmly, but comfortably, against the superior aspect of the proximal thighs. In addition, lumbar pad was located against the lower lumbar spine. The seat was adjusted so that the axis of the actuator arm was aligned with L5/S1 disc space. This was clinically identified by palpation of the posterior superior iliac spine (PSIS), which is at the level of S2, and then moving one inch superiorly. The upper part of the trunk was strapped to the back attachment with a belt. With the subject sitting erect, the force application straps were adjusted vertically with the second intercostal cartilage on the anterior chest wall. The head was stabilized neutrally on adjustable head rest (Fig. 1).
Each subject was positioned into an upright neutral starting position. This position was adjusted by ensuring that the anterior superior iliac spine and the PSIS were aligned in the horizontal plane [22]. The predetermined spinal range of motion, which was chosen to be the "target position" for participants during the testing protocol, was from neutral spinal posture to 30° lumbar flexion [23]. This angle was chosen so that it can be achieved by all subjects [9]. Each subject was asked to move into flexion as much as he/she can to determine the maximum available lumbar ROM and to determine whether he would be able to perform the experimental task. The dynamometer was locked in the 0° position to ensure the same starting position in the three testing trials for each participant.
The testing procedure started by a practice trial, where each participant was allowed to perform three repetitions of the test. Once each participant completed the practice trial, the standard test session started. Each participant was passively moved by the dynamometer and positioned in 30° of lumbar flexion for 10 seconds and they were instructed to remember the position, because they would be asked to reproduce this position (Fig. 1). Participants then returned to the neutral position and were instructed to reproduce the target position as accurately as they could. Participants reported to the tester when they felt the target position had been reached. Participants were required to hold the final position for three seconds and then a hold button was pressed so that the reproduced position was recorded. The test was repeated three times with a pre-adjusted rest period of 10 seconds in-between each trial. No verbal or visual feedback on performance was given to the subjects [8,22,24].
5. Data collection and statistical analysis
The absolute error (AE) values about the 30° target position were recorded for the three trials done by each participant and the mean deviation was calculated [25]. One way analysis of variance (ANOVA) and least significant difference (LSD) post hoc test were used to determine significant difference in the repositioning error between the groups across the measurements. SPSS ver. 13 (SPSS Inc., Chicago, IL, USA) were used to conduct the statistical analysis using an α level of 0.05. The study was granted ethical approval from the local Research Ethics Committee.
Results
1. Subjects' characteristics
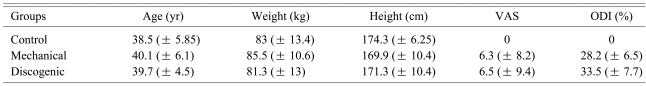
Forty five subjects participated in the study (32 males and 13 females). A summary of the demographic data of all participants is shown in Table 1. There was no significant difference among the three groups for age, weight and height. No significant difference was identified between MLBD and DLBD groups for VAS and ODI.
2. Repositioning accuracy
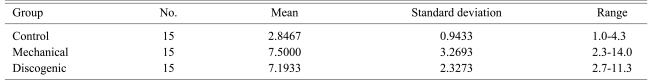
The AEs, measured in degrees, between the target and the reproduced position in the three testing trials were calculated for all subjects in the three groups. The average repositioning AEs were 2.8 (± 0.94), 7.5 (± 3.3) and 7.1 (± 2.3) degrees for the control, MLBD and DLBD groups, respectively. The average repositioning AE and ranges of the three groups are shown in Table 2.
3. Differences in repositioning accuracy between the three groups
ANOVA revealed significant difference between the mean values of the three groups (p < 0.0002). Lumbar repositioning AE values were significantly greater in the two LBD groups than in the control group. The healthy subjects repositioned their back more accurately to the target position, as shown by their average AE, while the LBD groups had a significantly larger AE. Application of the LSD post hoc test revealed significant difference in the repositioning AE between the control and the MLBD group (p < 0.0003), and between the control and the DLBD group (p < 0.0001). On the other hand, there were no significant differences in the repositioning AE between the non-specific mechanical and the discogenic LBD groups where the p-value was 0.73.
4. Correlation between pain and functional index and repositioning error
In order to investigate the association between the repositioning accuracy and the level of pain and functional capacity, Spearman correlation coefficients were calculated between the AE and the VAS and ODI values for the MLBD and DLBD groups. Correlation between AE and VAS has showed no association between them for both groups, where r = -0.043 and 0.225, for the MLBD and DLBD groups respectively. On the other hand, Spearman correlation coefficients showed weak association between AE and ODI, where r = 0.518 and 0.311, for the MLBD and DLBD groups respectively.
Discussion
The main aim of the present study was to compare the lumbar repositioning accuracy, as a measure of proprioception, in two different LBD populations compared to control subjects. The findings of the current study suggest that proprioception is affected in subjects with back dysfunction and that the proprioceptive deficit might constitute a part of the global dysfunction experienced by patients. The results of the study showed significant differences in the lumbar repositioning accuracy between the control and the two LBD groups. Lumbar repositioning AE were significantly greater in the LBD groups compared to the control group. The healthy subjects repositioned their back more accurately to the target position. However, no differences were found between the two LBD groups, showing that the proprioceptive deficits occur with the same degree regardless to the cause of the LBD whether mechanical or discogenic.
The difference in the lumbar repositioning accuracy between the control and the MLBD groups can be explained according to the essential basis of proprioception explained by Parkhurst and Burnett [17], where they stated that mechanoreceptors operate so that increased stretch or tension produces an increase in afferent signals, while impulses decrease with shortening. Accordingly, both increased and decreased muscle stretch may cause mechano-receptive dysfunction. In addition, the traditional view that joint receptors play the major role in controlling proprioception has been challenged in favour of the suggestion that muscle receptors may play an essential, perhaps primary, role [26]. Accordingly, it is assumed that muscle fatigue or shortening associated with LBD will have a drastic effect on the normal function of the muscle spindle, an important component for ensuring the correct positioning of the lumbosacral spine. Other explanation that may account for the results is that pain inhibition of local muscles such as lumbar multifidus may result in alterations in the normal muscle recruitment pattern resulting in the repositioning deficits [24].
Impaired postural control and lumbar proprioceptive deficits observed in patients with LBD were suggested to be a possible consequence of a feedback error resulting from sensory loss, information processing deficit, or both [21]. This may explain the differences in lumbar repositioning accuracy between the control and the DLBD groups. The non-significant difference between the two LBD groups suggest that the impaired position sense in both LBD groups can possibly be attributed to the fact that receptors important for proprioception are affected with dysfunction in the lumbar spine, and these proprioceptive deficits are not compensated by proprioceptive mechanisms outside the lumbar spine [9]. The instability concept in low back syndrome can provide another explanation for the proprioceptive deficits that occur with the same degree in the two LBD groups. The stability system of the spine consists of three components; the passive component (spinal column), the active component (spinal muscles) and the nervous component (neural control unit). Any overloading or disrupted function of any of these three components, as a result of mechanical or discogenic causes may lead to proprioceptive deficits and increased risk of injury [12].
The significant difference in the lumbar repositioning accuracy, which had been reported in this study, are in line with the earlier observations of Gill and Callaghan [9], who demonstrated that differences in proprioception do exist between individuals with LBP and those free from back pain. The findings were also in agreement with Taimela et al. [26], who noticed the presence of delayed lumbar muscle responses to sudden loads and impaired ability to sense a change in lumbar position as a result of paraspinal muscle fatigue. The results of this study is also supported by the earlier study conducted by Brumagne et al. [18], who suggested that patients with LBD may have proprioceptive disturbances possibly due to altered paraspinal muscle spindle afferents and impaired central processing of this sensory input. The findings were also supported by the study conducted by O'Sullivan et al. [24], who found that the inability of subjects with lumbar segmental instability to reposition the lumbar spine accurately into a neutral spinal posture is due to deficiency in lumbar proprioceptive awareness.
The findings of this study, however, differ from the earlier findings of Lam et al. [27] and Lee et al. [7], who failed to find significant difference in active lumbar repositioning accuracy between the study groups. This might be attributed to the inclusion of a heterogeneous (non-specific) LBD sample, which limited the ability to detect a difference between the study populations. Lee et al. [7] suggested, however, that impairments in proprioception do exist in individuals with back dysfunction, but it is better detected when assessed with a motion perception threshold measure.
The study done by Newcomer et al. [8] also failed to find difference between individuals with LBP and control subjects for the same reason, i.e., inclusion of a heterogeneous symptomatic study population, which may have limited their findings. In addition, the technique of measurement was not accurate enough. Testing the subjects in standing without immobilization of the legs provided extra-proprioceptive afferent input from the lower limbs and vestibular system. Newcomer et al. [28] repeated the same study, but with partial immobilization of the lower extremities and pelvis and they were able to detect a difference in the repositioning error that was not detected in the first study. The current study adopted the use of seated-compressed position, with adequate immobilization of the pelvis and the lower extremities, over the standing position because of its functional relevance and to minimize additional proprioceptive inputs from other distant receptors that have been noted in the standing position [24]. Also, in this position, the feet were held with no contact with the floor to minimize the proprioceptive input from the lower limbs. The current study included two particular subgroups of LBD patients, with distinctive inclusion/exclusion criteria and strict screening procedure, in order to recruit homogenous groups and to overcome limitations reported in previous studies.
The study has, however, been limited by several factors. First, the Biodex system 3 allows measuring the lumbar repositioning accuracy for movements in the sagittal plane only, i.e., lumbar flexion and extension, which limited the ability to measure the lumbar repositioning accuracy in side binding and rotation movements. In addition, the Biodex system 3 cannot measure fractions of degrees, which might have affected the accuracy of measurement. The main limitation is that the Biodex system 3 provided a considerable amount of sensory input due to large contact area with the body leading to increased cutaneous feedback.
It might be argued that the significant difference in the lumbar repositioning accuracy between the control and the two LBD groups can be attributed to the fact that spinal pain may result in coordination dysfunction during dynamic tasks, with alteration in the normal agonist-antagonist activity, particularly, as there is strong evidence to suggest that disturbances in neuromuscular control and motor performance may result directly from a reaction to the presence of pain [24]. However, during the current testing procedure, no subject reported severe pain in the back at the time of testing that might have interfered with the measurement. Furthermore, the results of the study showed weak correlation between pain and AE in the DLBD group (r = 0.225) while there was no correlation between pain and AE in the MLBD group (r = -0.043), which could eliminate any direct influence of pain on the study.
The study made significant contribution to the body of knowledge as it provided further evidence that proprioceptive dysfunction do exist in individuals with LBD. Moreover, the study is the first to compare two subgroups of LBD and investigate the difference in proprioceptive deficits between them. The study suggests that patients with LBD may have altered spinal proprioceptive function and disrupted joint position sense in the lumbar region compared to healthy individuals. The findings of the current study support the importance of incorporating a screening test for monitoring proprioceptive deficits in individuals with back dysfunction.
Conclusions
Differences in proprioception do exist between individuals with back dysfunction and normal subjects. Patients with back dysfunction had a less refined position sense than healthy individuals. The proprioceptive deficits do exist regardless of the cause of the back dysfunction, i.e., mechanical or discogenic, and may represent an important aspect of the patho-phsyiology of such a condition. Further research is needed to determine the different spinal lesions associated with a reduction in proprioception, and to determine whether such deficits can be corrected with specific exercise interventions and the role of proprioceptive retraining in the rehabilitation of back dysfunction.