|
 |
- Search
| Asian Spine J > Volume 9(2); 2015 > Article |
Abstract
Purpose
To evaluate the anatomy of the C2 lamina for translaminar screw placement based on computerized tomographic measurements.
Overview of Literature
C2 translaminar screw insertion is a novel technique for atlanto-axial fixation. The risk of vertebral artery injury can be decreased by this technique. However, a large series of anatomical studies on C2 anatomy in Asian populations is still lacking.
Methods
Two hundred adult C2 vertebrae were evaluated by computerized tomographic imaging. The measured parameters included inner and outer transverse diameters of C2 lamina, C2 laminar length and spino-laminar angle. C2 vertebrae with lamina screw placement feasibility were defined as those with inner transverse diameter larger than 3.5 mm.
Results
The mean inner transverse diameter of the C2 lamina was 4.23┬▒1.22 mm. It was significantly larger in males than in females (4.44┬▒1.29 mm vs. 3.96┬▒1.06 mm, p=0.005). The mean outer transverse diameter of C2 lamina was 6.64┬▒1.36 mm. The mean C2 laminar length was 37.26┬▒4.42 mm. The mean C2 spino-laminar angle was 56.42┬▒6.42 degrees. Seventy-nine percents of patients had inner transverse diameter larger than 3.5 mm.
Most of the instability in the upper cervical spine occurs at the atlantoaxial complex. Causes of instability can include congenital malformations, inflammatory diseases, infection, degenerative processes, neoplasms and trauma. The instability should be corrected to prevent further spinal cord damage.
Options for posterior fixation of the atlantoaxial complex include posterior wiring techniques, C1-C2 transarticular screw fixation, C1 lateral mass-C2 pars screw fixation and C1 lateral mass-C2 pedicular screw fixation.
Although wiring techniques are technically simple, their biomechanical limitations reduce fusion rates and necessitate rigid immobilization during the postoperative period [1]. C1-C2 transarticular screw fixation, C1 lateral mass-C2 pars screw fixation and C1 lateral mass-C2 pedicular screw fixation are very rigid. However, inherent in these techniques is the risk of injury to vertebral artery [2,3,4,5,6].
Wright [7] has recently reported on a series of patients with atlantoaxial instability in which a novel C2 fixation technique with bilateral crossing translaminar screws was used. This technique was reported to be relatively easy, rigid and reduces the risk of vertebral artery injury [8,9,10].
There are several reports in the literature discussing the anatomy of C2 lamina for translaminar screw placement [11,12,13,14,15,16,17,18]. However, most of these reports describe only the outer transverse diameter of the C2 lamina. The purpose of this study is to evaluate the anatomy of C2 lamina based on computerized tomographic measurements relative to C2 translaminar screw placement, with a focus on both the inner and outer transverse diameter of C2 lamina.
Two hundred cervical computerized tomographic (CT) images of adult patients at Ramathibodi Hospital between January 2008 and December 2012 were evaluated. The patients were randomly chosen from the patient registry. Patients who had C2 laminar abnormalities (e.g., fracture, infection or tumor) were excluded from the study. The C2 laminar parameters were measured from the CT images using the measurement tools of the workstation (Somatom Sensation cardiac 64, Siemens, Erlangen, Germany). One-millimeter thin CT images slices were cut parallel to the disc spaces.
The measured parameters for the C2 lamina include the smallest inner transverse diameter, the smallest outer transverse diameter, the C2 laminar length and spino-laminar angle. The C2 laminar length was measured from the base of the C2 spinous process to the junction between the C2 facet and lamina on the contralateral side (Fig. 1). The spino-laminar angle was defined as the angle between the sagittal plane and the axis of the C2 lamina (Fig. 2). The criterion for feasible C2 lamina screw placement was defined as the inner transverse diameter of the C2 lamina larger than 3.5 mm.
Statistical analysis was performed with the use of STATA version 11. Student's t-test was used to assess the level of statistical significance. Significance was defined as p-value <0.05.
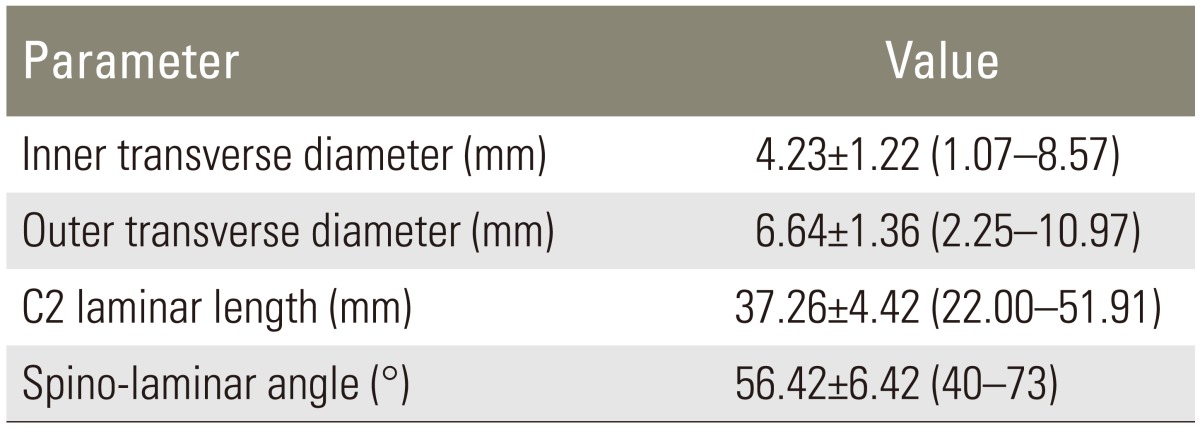
Two hundred patients were included in this study. There were 112 men and 88 women. The mean patient age was 53 years (range, 18-84 years). The mean inner transverse diameter of C2 lamina was 4.23┬▒1.22 mm. Seventy-nine percent of the patients had an inner transverse diameter larger than 3.5 mm. The mean outer transverse diameter was 6.64┬▒1.36 mm. The mean C2 laminar length was 37.26┬▒4.42 mm. The mean C2 spino-laminar angle was 56.42┬▒6.42 degrees (Table 1).
The inner transverse diameter of C2 lamina was significantly larger in males than in females (4.44┬▒1.29 mm vs. 3.96┬▒1.06 mm, p=0.005). When patients were stratified by age into 2 groups (Ōēż60 years vs. >60 years), there was no significant difference in age related to the inner transverse diameter of the C2 lamina (4.23┬▒1.29 mm vs. 4.22┬▒1.09 mm, p=0.94) (Table 2).
Posterior fixation of C1-C2 subluxation has been performed with a variety of techniques including posterior wiring techniques, C1-C2 transarticular screw fixation, C1 lateral mass-C2 pars screw fixation and C1 lateral mass-C2 pedicular screw fixation. Transarticular screw technique, C1 lateral mass-C2 pars screw fixation and C1 lateral mass-C2 pedicular screw fixation are very rigid but contain a risk of vertebral artery injury [2,3,4,5,6].
For this reason, Wright [7] proposed a method using bilateral crossing of C2 translaminar screws in atlantoaxial fusion. The major advantage of this technique is elimination of the potential risk of vertebral artery injury by placing screws within the C2 lamina. Other advantages include the relative ease of the technique and sufficient rigid stability [8,9,10]. Dorward and Wright [19] reported 97% fusion rate in their series with this technique.
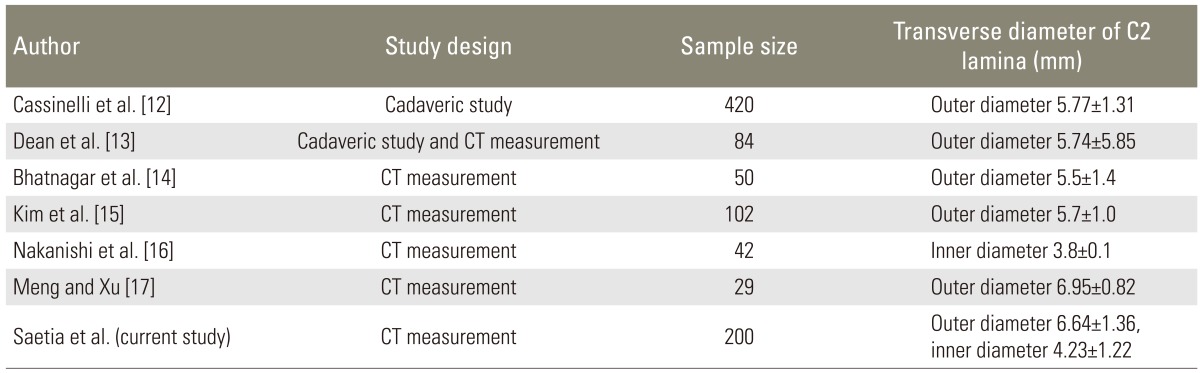
The anatomy of C2 lamina for translaminar screw placement has been studied in the literature. Most studies described only the mean outer transverse diameter of the C2 lamina, which varies from 5.5 to 6.95 mm [12,13,14,15,17,18]. In this study, the mean outer transverse diameter of the C2 lamina was 6.64 mm, which is comparable to other reports.
There is limited data in the literature regarding the inner transverse diameter of the C2 lamina. Nakanishi et al. [16] evaluated CT scans of the C2 lamina in 42 Japanese patients. The mean inner transverse diameter of C2 lamina was 3.8 mm compared to 4.23 mm in this study. This variation might be from ethnic differences. Literature describing the transverse diameter of C2 lamina for translaminar screw placement is summarized in Table 3.
In this study, the mean inner transverse diameter of C2 lamina was significantly larger in males than in females (4.44┬▒1.29 mm vs. 3.96┬▒1.06 mm, p=0.005). This gender difference in C2 lamina diameter has been reported by several authors [12,15,16]. Nakanishi et al. [16] reported that the mean inner transverse diameter of C2 lamina in males and in females was 4.1 mm and 3.5 mm, respectively. In the study by Kim et al. [15], the mean outer transverse diameter of C2 lamina in males and in females was 5.8 mm and 5.4 mm, respectively.
Seventy-nine percent of the population in this study had C2 anatomy that was suitable for C2 translaminar screw placement. In the literature, the percentage of C2 lamina appropriate for this technique varied from 50 to 100 percent [11,14,15,16,17]. Meng and Xu [17] studied 29 adult patients with os odontoideum. All patients had C2 lamina with diameters suitable for translaminar screw placement. However, another study by Yusof and Shamsi [18] found that the C2 lamina in the Malaysian population is relatively small. The mean outer transverse diameter was 5.6 mm. They suggested that C2 translaminar fixation using a 3.5 mm screw should be attempted with caution in the Asian population.
Conflict of Interest
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
References
1. Lapsiwala SB, Anderson PA, Oza A, Resnick DK. Biomechanical comparison of four C1 to C2 rigid fixative techniques: anterior transarticular, posterior transarticular, C1 to C2 pedicle, and C1 to C2 intralaminar screws. Neurosurgery 2006;58:516ŌĆō521. PMID: 16528192.



2. Lau SW, Sun LK, Lai R, et al. Study of the anatomical variations of vertebral artery in C2 vertebra with magnetic resonance imaging and its application in the C1-C2 transarticular screw fixation. Spine (Phila Pa 1976) 2010;35:1136ŌĆō1143. PMID: 20118834.


3. Madawi AA, Casey AT, Solanki GA, Tuite G, Veres R, Crockard HA. Radiological and anatomical evaluation of the atlantoaxial transarticular screw fixation technique. J Neurosurg 1997;86:961ŌĆō968. PMID: 9171174.


4. Wright NM, Lauryssen C. Vertebral artery injury in C1-2 transarticular screw fixation: results of a survey of the AANS/CNS section on disorders of the spine and peripheral nerves. American Association of Neurological Surgeons/Congress of Neurological Surgeons. J Neurosurg 1998;88:634ŌĆō640. PMID: 9525707.


5. Gluf WM, Schmidt MH, Apfelbaum RI. Atlantoaxial transarticular screw fixation: a review of surgical indications, fusion rate, complications, and lessons learned in 191 adult patients. J Neurosurg Spine 2005;2:155ŌĆō163. PMID: 15739527.


6. Neo M, Fujibayashi S, Miyata M, Takemoto M, Nakamura T. Vertebral artery injury during cervical spine surgery: a survey of more than 5600 operations. Spine (Phila Pa 1976) 2008;33:779ŌĆō785. PMID: 18379405.


7. Wright NM. Posterior C2 fixation using bilateral, crossing C2 laminar screws: case series and technical note. J Spinal Disord Tech 2004;17:158ŌĆō162. PMID: 15260101.


8. Matsubara T, Mizutani J, Fukuoka M, Hatoh T, Kojima H, Otsuka T. Safe atlantoaxial fixation using a laminar screw (intralaminar screw) in a patient with unilateral occlusion of vertebral artery: case report. Spine (Phila Pa 1976) 2007;32:E30ŌĆōE33. PMID: 17202877.


9. Gorek J, Acaroglu E, Berven S, Yousef A, Puttlitz CM. Constructs incorporating intralaminar C2 screws provide rigid stability for atlantoaxial fixation. Spine (Phila Pa 1976) 2005;30:1513ŌĆō1518. PMID: 15990665.


10. Lehman RA Jr, Dmitriev AE, Helgeson MD, Sasso RC, Kuklo TR, Riew KD. Salvage of C2 pedicle and pars screws using the intralaminar technique: a biomechanical analysis. Spine (Phila Pa 1976) 2008;33:960ŌĆō965. PMID: 18427316.


11. Ma XY, Yin QS, Wu ZH, Xia H, Riew KD, Liu JF. C2 anatomy and dimensions relative to translaminar screw placement in an Asian population. Spine (Phila Pa 1976) 2010;35:704ŌĆō708. PMID: 20195212.


12. Cassinelli EH, Lee M, Skalak A, Ahn NU, Wright NM. Anatomic considerations for the placement of C2 laminar screws. Spine (Phila Pa 1976) 2006;31:2767ŌĆō2771. PMID: 17108826.


13. Dean CL, Lee MJ, Robbin M, Cassinelli EH. Correlation between computed tomography measurements and direct anatomic measurements of the axis for consideration of C2 laminar screw placement. Spine J 2009;9:258ŌĆō262. PMID: 18757247.


14. Bhatnagar R, Yu WD, Bergin PF, Matteini LE, O'Brien JR. The anatomic suitability of the C2 vertebra for intralaminar and pedicular fixation: a computed tomography study. Spine J 2010;10:896ŌĆō899. PMID: 20615759.


15. Kim YJ, Rhee WT, Lee SB, You SH, Lee SY. Computerized tomographic measurements of morphometric parameters of the c2 for the feasibility of laminar screw fixation in Korean population. J Korean Neurosurg Soc 2008;44:15ŌĆō18. PMID: 19096651.



16. Nakanishi K, Tanaka M, Sugimoto Y, et al. Application of laminar screws to posterior fusion of cervical spine: measurement of the cervical vertebral arch diameter with a navigation system. Spine (Phila Pa 1976) 2008;33:620ŌĆō623. PMID: 18344855.


17. Meng XZ, Xu JX. The options of C2 fixation for os odontoideum: a radiographic study for the C2 pedicle and lamina anatomy. Eur Spine J 2011;20:1921ŌĆō1927. PMID: 21725866.



18. Yusof MI, Shamsi SS. Translaminar screw fixation of the cervical spine in Asian population: feasibility and safety consideration based on computerized tomographic measurements. Surg Radiol Anat 2012;34:203ŌĆō207. PMID: 21947622.


19. Dorward IG, Wright NM. Seven years of experience with C2 translaminar screw fixation: clinical series and review of the literature. Neurosurgery 2011;68:1491ŌĆō1499. PMID: 21346648.



Fig.┬Ā1
Axial computerized tomographic image illustrates the measurement of C2 inner transverse diameter (a), C2 outer transverse diameter (b) and C2 laminar length (c).
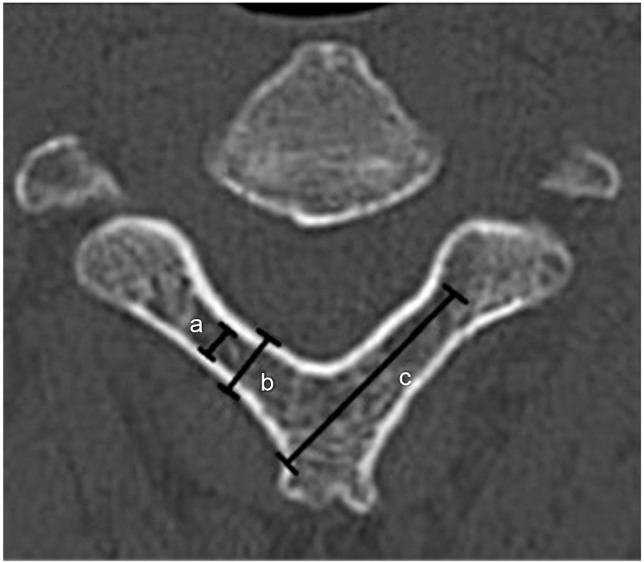
Fig.┬Ā2
Axial computerized tomographic image illustrates the measurement of C2 spino-laminar angle (d).