 |
 |
- Search
| Asian Spine J > Volume 17(3); 2023 > Article |
|
Abstract
The present systematic review and meta-analysis was conducted to compare the safety and efficacy of the two approaches for primary spinal cord tumors (PSCTs) in adult patients (laminoplasty [LP] vs. laminectomy [LE]). LE is one of the most common procedures for PSCTs. Despite advantages of LP, it is not yet widely used in the neurosurgical community worldwide. The efficacy of LP vs. LE remains controversial. Adult patients over 18 years of age with PSCT at the level of the cervical, thoracic, and lumbar spine were included in the study. A literature search was performed in MEDLINE via PubMed, EMBASE, The Cochrane Library, and Google Scholar up to December 2021. Operation time, hospital stay, complications, and incidence of postoperative spinal deformity (kyphosis or scoliosis were extracted. A total of seven retrospective observational studies with 540 patients were included. There were no significant differences between LP and LE group in operation time (p=0.25) and complications (p=0.48). The LE group showed larger postoperative spinal deformity rate than the LP group (odds ratio, 0.47; 95% confidence interval [CI], 0.27ŌłÆ0.84; p=0.01). The LP group had a shorter hospital stay (standardized mean differences, ŌłÆ0.68; 95% CI, ŌłÆ1.03 to ŌłÆ0.34; p=0.0001) than the LE group. Both LP and LE have comparable operative times and total complications in the treatment of PSCT. LP was superior to LE in hospital stay and postoperative spinal deformity rate. However, these findings are limited by the very low quality of the available evidence. Randomized controlled trials are needed for further comparison.
Primary spinal cord tumors (PSCTs) include intradural intramedullary tumors developing from the cellular elements of the spinal cord, as well as intradural extramedullary tumors such as schwannomas and meningiomas, that do not originate from the cord [1]. Extramedullary tumors are formed from peripheral nerve roots or their membranes and are not part of the central nervous system (CNS), whereas intramedullary tumors originate from glial and support cells of the spinal cord. In this meta-analysis, the term ŌĆ£PSCTŌĆØ will be used to designate all intramedullary and extramedullary (intradural and extradural) pathologies within the spinal canal arising from glial cells and supporting cells [2].
PSCTs account for about 4%ŌĆō8% of tumors that occur in the CNS. They are more common in adults than in children (mean age=51 years) and are often benign [3]. When the tumor causes compression of neural structures, damage to the spinal cord and spinal roots occurs. The most common histological types of PSCT are meningiomas, schwannomas, and ependymomas [3]. Surgical resection remains the primary curative option for PSCT [1].
Laminectomy (LE) is the most widely used procedure for removing PSCTs [4,5]. However, LE may be associated with segmental instability, postoperative spinal deformity (kyphosis and scoliosis), and epidural scar formation; as a result, a high frequency of reoperations is observed [5ŌĆō8].
Laminoplasty (LP), which can be considered as an alternative to LE in PSCT, is popularized by Japanese orthopedic surgeons for posterior decompression in degenerative cervical myelopathy. There are more than 20 variations of LP. The most commonly used LP techniques are modifications of the open-door LP (developed by Hirabayashi and colleagues in 1977) and the double-door LP (described by Kurokawa and colleagues in 1982) [5]. LP allows access for tumor removal, followed by restoration of the spinal ring (when mini-plates of grafts are used) and provides a dorsal roof for the spinal cord [4,5].
Despite the benefits of LP, it has not yet been widely accepted by the neurosurgical community and has not become the gold standard treatment for PSCT. The lack of information on the efficacy of LP in the treatment of PSCT, as well as contradictory data comparing LP with LE, was the motivating factors for this meta-analysis.
This meta-analysis was conducted to systematically compare the safety and efficacy of the two posterior approaches for PSCTs of adult patients (LP versus LE) to address limitations in the current literature.
This review followed PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) [9] guidelines and AMSTAR (A Measurement Tool to Assess Systematic Reviews) 2 [10] appraisal tool. A systematic search was conducted through MEDLINE via PubMed, Cochrane Library, EMBASE, and Google Scholar databases. A highly sensitive search strategy using the keywords ŌĆ£laminoplastyŌĆØ and ŌĆ£spinal tumorŌĆØ or ŌĆ£primary spinal cord tumorŌĆØ or ŌĆ£oncologyŌĆØ or ŌĆ£extramedullary tumorŌĆØ or ŌĆ£intramedullary tumorŌĆØ or ŌĆ£intradural tumorŌĆØ was performed. A broad search strategy using only the keyword ŌĆ£laminoplastyŌĆØ was also performed. Irrelevant studies were excluded and duplicates were removed. Only original articles from 1980 to 2021 were selected. Additional references were found by manually searching literature lists of relevant studies, conference abstracts, registered clinical trials, and by contacting experts in the field. The search was limited to publications in English.
All the articles were selected using the previously stated keywords. The data were selected independently by two authors (R.P., A.K.), who checked all relevant titles and abstracts of publications to exclude irrelevant ones. Researchers independently evaluated full reports, after which each selected article was independently evaluated by the entire author team using the PICOS (Population, Intervention, Comparison, Outcome, Study Design) [11] inclusion and exclusion criteria (Table 1) [12].
Data were extracted independently by two reviewers (R.P. and A.K.). The data included the following: study design, patients (age, sex, and tumor type), type of surgery (LP and LE), LP technique, clinical (clinical scales, complications, blood loss, and operation time), and radiological outcomes (postoperative kyphotic deformation). As all studies included were nonrandomized controlled retrospective studies, the Newcastle-Ottawa Scale was used to assess the quality of each study [13].
The study analyzed the following data primarily: (1) operation time, (2) hospital stay, and (3) complications. The incidence of postoperative spinal deformity, which was defined as loss of cervical or lumbar lordosis, appearance or worsening (>10┬░ Cobb angle) of cervical or thoracic kyphosis, or new appearance or worsening of scoliosis were also analyzed.
Review Manager ver. 5.3 (The Nordic Cochrane Center, The Cochrane Collaboration, Copenhagen, Denmark) was used for data analysis. Risk ratio (RR), odds ratio (OR), and 95% confidence interval (CI) were calculated for dichotomous variables; standardized mean differences (SMD) and their 95% CI were used for continuous variables. The degree of heterogeneity was assessed using the I2 coefficient. A fixed-effects model was used for no heterogeneity, and a random-effects model was used if I2 was more than 40%. A funnel plot was constructed and the Egger test was performed to assess publication bias. A p-value <0.05 was utilized to indicate statistical significance.
Fig. 1 shows a summary of the study selection process. A total of 2,717 articles were identified through MEDLINE, Cochrane Library, EMBASE, and Google Scholar databases. A total of 2,631 studies were excluded as they were duplicates, irrelevant studies, case reports, and review. A total of 86 potential articles were retrieved for further full-text evaluation. Among them, 61 articles were excluded for not meeting the inclusion criteria. Finally, 25 studies were included in the qualitative synthesis and seven studies with 540 patients were included in this meta-analysis. Table 2 summarizes the main characteristics of the included studies [14ŌĆō38].
Seven studies were included in this meta-analysis. These studies were published between 1996 and 2021. The number of patients in the LP and LE group was 194 and 346, respectively. As all studies were retrospective nonrandomized studies, the Newcastle-Ottawa Scale was used to assess the quality. The quality of each study was low and medium (Table 2).
Operative time was analyzed in two studies (51 patients in the LP group and 51 patients in the LE group) [18,25]. Both groups showed similar operative times (SMD, ŌłÆ0.44; 95% CI, ŌłÆ1.18 to 0.31; čĆ=0.25; I2=71%; random-effect model) (Fig. 2). The average operative time was 157.71 minutes in the LP group and 175.3 minutes in the LE group.
Four studies reported information about hospital stay of LP (n=128) and LE (n=254) [18,23,25,29]. The LP group showed shorter hospital stays (SMD, ŌłÆ0.68; 95% CI, ŌłÆ1.03 to ŌłÆ0.34; čĆ=0.0001; I2=48%; random-effect model) than the LE group (Fig. 3). The average hospital stay was 7.8 days and 11.3 days, in the LP and LE groups, respectively.
Five studies reported complications after LP (n=162) and LE (n=314) [14,18,23,25,29]. There were 17/162 (10.4%) complications in the LP group and 43/314 (13.6%) in the LE group. Total complications were similar between the two groups (RR, 0.83; 95% CI, 0.50ŌłÆ1.38; čĆ=0.48; I2=0%; fixed-effect model) (Fig. 4).
Postoperative spinal deformity rate was analyzed in six studies [14,18,25,29,35,38]. The overall rate of postoperative spinal deformity was statistically significantly lower (OR, 0.47; 95% CI, 0.27ŌłÆ0.84; čĆ=0.01; I2=6%; fixed-effect model) in patients who underwent LP (21/175 [12%]) than in those who underwent LE (58/323 [18%]) (Fig. 5).
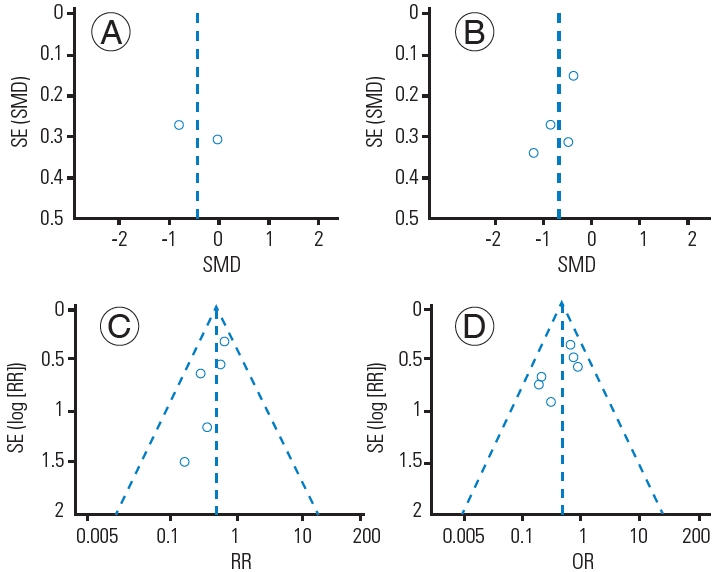
Assessment of publication bias for each parameter of the included studies was performed by funnel plots on visual inspection. The studies were nearly symmetrically distributed on both sides of the vertical line, indicating a relatively small publication bias (Fig. 6). However, there were fewer than 10 studies in the meta-analysis and the test power was too low to distinguish chance from real asymmetry.
The LP technique was developed for the purpose of decompressing the spinal canal for degenerative and inflammatory conditions, while retaining the dorsal structures [5]. The spinal cord remains exposed following LE, whereas the spinal ring can be recreated fully and the spinal cord can be covered with LP. LP has not been widely used in PSCT surgery, where the canal itself is usually not narrowed relative to the spinal cord once the tumor has been removed.
Most scientific papers suggest that the resection of ligaments, facet joints, and laminae is accompanied by an increase in the range of motion (ROM) and a decrease in the stability of the operated segments [39]. Healy et al. [40], when analyzing the biomechanics of open-door LP, demonstrated that LE, as compared to LP, led to a relatively greater increase in global cervical ROM. An increase in segmental ROM may be a factor in the occurrence of postoperative pain syndrome and the risk of postoperative spinal deformity. Subramaniam et al. [41] noted, using cadavers, the advantage of LP over LE in maintaining spinal stability: ROM after LE was 13% greater than after LP. Despite ample evidence from biomechanical studies [42], including those using computer modeling and finite element analysis [43], the results of the clinical use of LP in PSCT surgery remain uncertain. This may be because of the wide variety of LP techniques in PSCT surgery, which is supported by the data from published studies included in our systematic review. The literature lacks definitive information on several aspects of using LP for PSCT surgery, including the adequacy of intraoperative visualization of and access to the tumor, the ability to resect the entire mass, the size of the mass that can be resected, the postoperative clinical and radiological results.
In the present meta-analysis, patients in the LP group had significantly shorter hospital stays compared to LE. The exact reasons are not clear, but it may be conjectured that reconstruction of the posterior elements somehow results in a decrease in postoperative pain, or an improvement in neurological symptoms, allowing early mobilization. The reason needs to be investigated in prospective studies with sufficient power, using validated clinical scales and measuring the time of mobilization for the two groups.
A statistically significantly lower incidence of postoperative spinal deformity in the LP group was found as compared to the LE group. This may be caused by the restoration of the posterior elements, to which extensor muscles can attach and pull. Spinous processes elevate the extensor mechanism away from the center of rotation of the spine, thereby increasing the biomechanical moment arm of the pulling force. In contrast, with LE, the extensor mechanism has nothing to attach to and, without spinous processes to hold it up, it is functionally elongated, increasing the risk of postoperative spinal deformity. The findings of the present study were consistent with the results of the series by McGirt et al. [29] with a follow-up period of up to 2 years, where the advantage of LP was confirmed: Following LP versus LE, 5 (9%) versus 21 (12%) patients developed progressive deformity (p=0.728) at a mean of 14 months after surgery. A thorough assessment of all factors that influence the deformity is needed: the degree of facet joint resection, the number of levels of decompression, the severity of the initial degenerative changes, the presence of preoperative spinal instability, systemic diseases of the connective tissue, etc. Additional studies are required to know the biomechanical features and reconstructive nature of LP for the prevention of postoperative spinal deformity.
There were no statistically significant differences between the groups with respect to the duration of surgery and the risk of postoperative complications. This suggests that LP may be advantageous, since it restores the vertebral structures following tumor removal, but it is not associated with an increased risk of complications or significantly increased operative times. In five of the retrospective studies, all postoperative complications were identified without specifying which ones were related to LP or LE. Likewise with perioperative complications, most studies failed to specify which complications were associated with LP versus LE groups.
To date, there is a single meta-analysis by Sun et al. [44], which is devoted to the subject of this study. The authors evaluated 16 studies with a total of 1,096 patients with PSCT treated with LP or LE. Statistically significant differences were noted between both groups in terms of effective recovery rate (p=0.003), blood loss (p<0.00001), hospital stay (p=0.006), postoperative spinal deformity (p=0.01), and cerebrospinal fluid leak (p<0.00001). However, there were no significant differences in the total resection rate of tumors (p=0.21) and operative time (p=0.14). In a subgroup analysis, the results indicated that age, type of tumor, follow-up period, surgical levels, and methods were associated with an increased incidence of postoperative spinal deformity [44]. Despite the seemingly clear advantages of LP over LE, a meta-analysis by Sun et al. [44] has a number of significant methodological problems. First, the final synthesis included both children and adults. The efficacy of LP in the pediatric population is well known and confirmed in studies with long follow-up [29,45,46], which could significantly bias the results in favor of LP when clubbing adults and children together. The present study, therefore, considered to evaluate LP in adult patients. Secondly, a meta-analysis by Sun et al. [44] included a large number of clinical studies written in Chinese, which complicates methodological evaluation and analysis of primary texts that are not in the public domain. Thirdly, the authors did not include a number of studies that the present study used as search strategy that met their inclusion criteria [14,18,23,35,38]. This indicated that their systematic search and selection of papers were incomplete. This study was unable to conduct a meta-analysis on many parameters because of lack of sufficient data, in contrast to the work of Sun et al. [44], where the advantages of LP are more definitively identified.
If the significant number of methodological shortcomings in the design of the included publications were considered, this study results indicate the need for further research aimed at the clinical and radiological efficacy of LP in PSCT surgery in adults. The published series could not analyze the most advantageous method based on the exact location of the tumor.
There are several fundamental limitations to this study. First, it concerns the design of the studies included in the meta-analysis. There are no prospective randomized trials on this topic. All the included studies were of a retrospective observational nature with no blinding procedure. There are many biases including selection bias, attrition bias, reporting bias, and other systematic and random errors. Second, a small number of subjects in each of the studies, or lack of data, confounded our statistical analyses, although this was partially mitigated by the meta-analysis itself. The CI for postoperative spinal deformity crossed the central axis in many studies. There was no distinction between the occurrence of postoperative kyphotic and scoliotic deformities. Therefore, a general term ŌĆ£postoperative spinal deformity,ŌĆØ was used in this study that included both scoliosis and kyphosis cases. Assessment of deformity in degrees was presented only in one paper, which precluded us from presenting a meta-analysis of the degree of deformity for both groups. Although hospital length of stay was statistically significant, there was a fairly high degree of heterogeneity (I2=64%). Significant variation, and, in some cases, the lack of necessary data, precluded us from performing a meta-analysis on parameters such as blood loss, total resection rate, etc., as the effectiveness of LP using validated clinical scales such as McCormick, Japanese Orthopaedic Association, 36-item Short Form Health Survey, Visual Analog Scale, and so forth. A number of studies had high heterogeneity within groups. For example, Song et al. [18] included patients who underwent LE with instrumented arthrodesis, instead of putting them into a separate subgroup. Tatter et al. [15] reported no details regarding postoperative kyphotic deformity, only two cases required revision stabilization. All of the above discrepancies likely affected our analyses of the duration of surgery, hospital stay, the frequency of postoperative complications, and the risk of postoperative spinal deformity. Third, the inclusion of studies performed on different regions of the spine in the meta-analysis is an important limitation when determining the incidence of postoperative spinal deformity. The incidence of deformity is highly dependent on the spinal region; in our opinion, combining all data without taking this factor into account introduces significant biases and complicates the unambiguous interpretation of the meta-analysis. Finally, another potential limitation of this study is that it only analyzed studies published in English.
The study revealed significant advantages of LP compared to LE in PSCT surgery. The LP procedure had a shorter hospital stay and a lower incidence of postoperative spinal deformity, with comparable operative times and surgical complications. The advantages of LP include prevention of adhesion of the dura to the paravertebral tissues, reconstruction of the dorsal roof of the spinal canal, and restoration of the spinal ring. It also results in early mobilization, a faster return to previous physical activity, and, likely, a lower risk of postoperative spinal deformity. If our analysis would be verified with future studies, we believe that LP should be adopted as the approach of choice for PSCT surgery, since it retains normal anatomy and is less invasive than LE [47].
Clinical trial data obtained from meta-analyses are highly susceptible to biases because of small sample sizes and the retrospective nature of the studies. Therefore, it is necessary to conduct large, prospective, randomized clinical trials with long-term follow-up, using a uniform LP technique to preserve the original spinal canal diameter, to improve the methodological quality of studies, as well as to objectively compare LP to LE.
Notes
Author Contributions
Conception and design: VB, RP; data acquisition: VB, RP, AK, MK, VS, ES; analysis of data: VB, RP, AK, EB, VS, VM; drafting of the manuscript: VB, RP, AK, MK, VS, EES; critical revision: VB, KDR; obtaining funding: none; administrative support: VB; supervision: KDR; and final approval of the manuscript: all authors.
Fig.┬Ā1
Flow diagram of the studies included in the systematic review according to PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses).

Fig.┬Ā2
Forest plots of operative time in laminoplasty and laminectomy groups. SD, standard deviation; SMD, standardized mean difference; IV, inverse variance; CI, confidence interval; df, degrees of freedom.
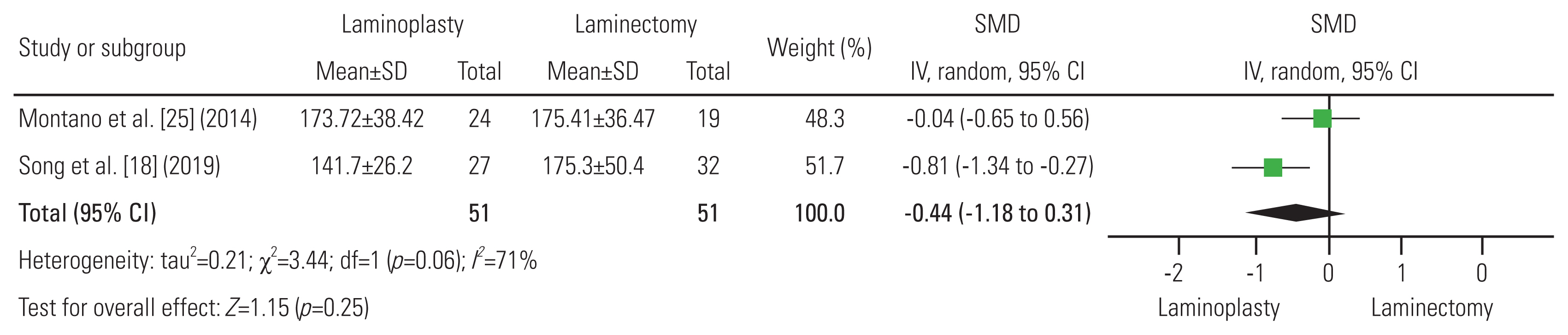
Fig.┬Ā3
Forest plots of hospital stay in laminoplasty and laminectomy groups. SD, standard deviation; SMD, standardized mean difference; IV, inverse variance; CI, confidence interval; df, degrees of freedom.

Fig.┬Ā4
Forest plots of total complications in laminoplasty and laminectomy groups. M-H, Mantel-Haenszel; CI, confidence interval; df, degrees of freedom.
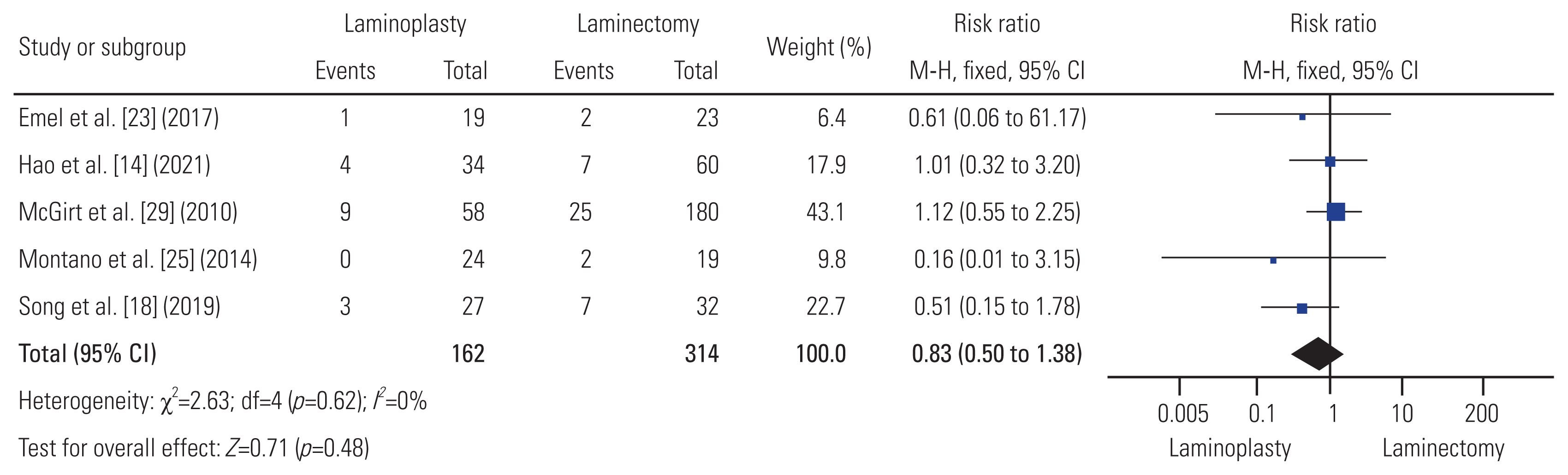
Fig.┬Ā5
Forest plots of postoperative spinal deformity rate in laminoplasty and laminectomy groups. M-H, Mantel-Haenszel; CI, confidence interval; df, degrees of freedom.
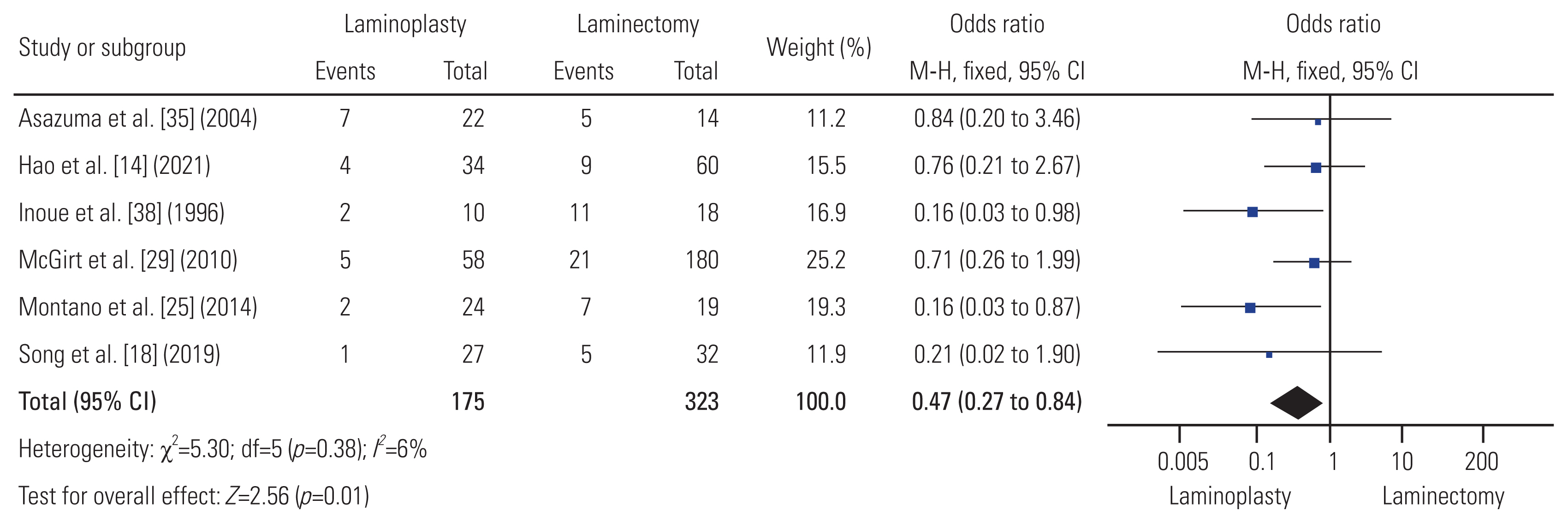
Fig.┬Ā6
Funnel plots for: operative time (A), hospital stay (B), complication (C), and postoperative spinal deformity rate (D). SE, standard error; SMD, standardized mean difference; RR, risk ratio; OR, odds ratio.
Table┬Ā1
PICOS: inclusion and exclusion criteria
| PICOS element | Inclusion criteria | Exclusion criteria |
|---|---|---|
| Population | - Adult patients over 18 years of age with PSCT at the level of the cervical, thoracic, lumbar spine, amenable to removal from the posterior approach |
- Children under 18 years of age - PSCT located above the level of the C2 - Primary tumors of the spine - Metastatic lesions of the spine and spinal cord - Tumors in the sacral spine - Primary ŌĆ£dumbbellŌĆØ tumors types 2ŌĆō4 according to the Eden classification [12] |
| Intervention | - ŌĆīAccess to the spinal canal using various modifications of LP |
- LP performed at a level above C2 - Ventral approaches - Corpectomy - Lateral approaches - Costotransversectomy |
| Comparison | - Traditional laminectomy |
- Hemilaminectomy - Translaminar approach |
| Outcome | - ŌĆīOutcome measures including primary and secondary outcomes | - None |
| Study design | - ŌĆīRandomized controlled trials, non-randomized prospective and retrospective observational studies |
- Single case reports - Systematic reviews, meta-analyses - Nonclinical trials |
| Publications | - Full-text publications in English | - ŌĆīPublications in other languages, unpublished studies, protocols, conference and presentation materials, abstracts, surgical videos |
Table┬Ā2
General characteristics of the studies included in the systematic review and meta-analysis
| Reference | Study design | Details of participants | Tumor type | LP type and level | Follow-up (mo) | Main results | Complications (events per sample) | Newcastle-Ottawa score |
|---|---|---|---|---|---|---|---|---|
| Hao et al. [14] (2021) | Retrospective cohort study | Mean age: 45 yr; LP (n=34), LE (n=60); M (n=58), F (n=36) | Ependymoma; low-grade astrocytoma; malignant astrocytoma; cavernoma; schwannoma; angiolipoma; meningioma; neurofibroma; epidermoid cyst; enterogenous cysts; epidural simple cyst | LP with screws and connectors; cervical, thoracic, lumbar | 12 | No significant difference between the LE and LP in terms of operative time, infection, CSF leak, and length of hospitalization (p>0.05). The incidence of postoperative spinal deformity was 15.0% in the LE and 11.7% in the LP (p>0.05). LP vs. LE was associated with a similar risk of progressive deformity. For the cervical subgroup, there is significant difference (p<0.05) in postoperative spinal deformity. | LP 4/34; LE 7/60 | ***/**/*** |
| Tatter et al. [15] (2020) | Retrospective cohort study | Mean age: 52 yr; LP (n=34), LE (n=50); M (n=37), F (n=75) | Ependymoma; hemangioblastoma; meningioma; neurofibroma; schwannoma; other; intradural chordoma; hemangiopericytoma; histology inconclusive; intramedullary lipoma; neurilemmoma; neurothekeoma; dermoid | LP with miniplates; cervical | 47┬▒36 | Two patients (2.4%) required delayed posterior fixation. The mean radiological kyphotic increase after surgery was 3.0┬░, which was significantly associated with LE of C2 and C3. Of these, C3 LE demonstrated independent risk association. | Not divided into groups: 1/84 | ***/**/*** |
| Kumar et al. [16] (2020) | Retrospective case series | Mean age: 35.28 yr; LP (n=14); M (n=5), F (n=9) | Schwannoma; meningioma; ependymoma; lymphoma; neurofibroma; teratoma | Flipped reposition LP technique; thoracic, lumbar | 17 (6ŌĆō26) | Two patients were assessed with ASIA grade A neurology, one patient improved to grade B, whereas the other did not improve. Two patients improved from grade B to grade D, and seven patients with grades C and D improved to grade E. Fusion at the osteotomy site was seen in 92.85% (13 out of 14 cases) on one side within 6 months postoperation. Fusion was seen in all the cases within 1-year postoperation. | LP 2/14 | NA |
| Cofano et al. [17] (2020) | Retrospective cohort study | Mean age: 58 yr; LP (n=23), LE (n=226); M (n=88), F (n=161) | Schwannoma; meningioma; ependymoma; paraganglioma; neurofibroma; hemangiotelioma; hemangiopericitoma; dermoid cyst; epidermoid cyst | Laminotomy with ultrasonic aspirator; LP with titanium screws and plates; cervical, thoracic, lumbar | 48.3 | Functional outcomes were not associated with the approach. No associations were seen between surgical approach and the incidence of incidental durotomy or the degree of resection. Minimally invasive approaches (monolateral LE) resulted to be equally effective for tumor resection compared to bilateral LE or LP and no major complications were observed (e.g., revisions for dural leakage). | Not divided into groups: 19/249 | ***/**/*** |
| Song et al. [18] (2019) | Retrospective cohort study | Mean age: LP (53.3 yr), LE (49.4 yr); LP (n=27), LE (n=32); M (n=27), F (n=32) |
LP group: Meningioma; Neurilemmoma; Neurofibroma; Lipoma; Ependymoma LE group: Neurilemmoma; Neurofibroma; Ependymoma; Meningioma; Lipoma; Neuroepithelial cyst |
LP with with a reconstruction plate (Fuller Inc., Beijing, China); thoracic, lumbar | 12 | Patients in the LP group had lower blood loss (LP: 281.5┬▒130.2 mL; LE: 450.0┬▒224.3 mL; p=0.001), shorter surgical time (LP: 141.7┬▒26.2 min, LE: 175.3┬▒50.4 min; p=0.003), lower volume of drainage (LP: 1,578.9┬▒821.7 mL; LE: 2,621.2┬▒1,351.0 mL; p=0.001), shorter drainage time (LP: 6.6┬▒2.5 days; LE: 9.7┬▒1.8 days; p=0.000), and a shorter hospital stay (LP: 16.9┬▒4.9 days; LE: 21.0┬▒4.4 days; p=0.002) compared with patients in the LE. There were significant differences of ODI between the two groups. The incidence of secondary spinal stenosis in the LP was significantly reduced (p=0.029). | LP 3/27; LE 7/32 | ***/**/*** |
| Onyia et al. [19] (2018) | Retrospective cohort study | Mean age: 40.6 yr; LP (n=24), LE (n=36); M (n=37), F (n=23) | Arachnoid cyst; hamartoma; hemangioblastoma; meningioma; neurofibroma; schwannoma; astrocytoma; ependymoma I; ependymoma II; ependymoma III; ganglion-cell tumor/paraganglioma; glomerular basal membrane; tuberculosis granuloma; plasma cell granuloma; other inflammatory lesions (nonspecific); lipoma; drop metastasis | Not reported; cervical, thoracic, lumbar | Mean LP (21), LE (13.1) | The incidence of neurologic function remaining unchanged at the end of follow-up was similar between LP and LE (12.5% vs. 11.1%). LP not more or less likely to have any better functional outcome or need for revision compared to LE in the resection of longŌĆÉsegment intradural lesions. | None | ***/**/*** |
| Miyakoshi et al. [20] (2018) | Retrospective case series | Mean age: 76 yr, 60 yr; LP (n=2); M (n=1), F (n=1) | Schwannoma | Open-door LP with hydroxyapatite spacers; cervical | 72 | Both patients showed a combination of spondylotic changes in the cervical spine and stenosis at the level of the tumor. Both tumors were successfully resected through open-door LP with hydroxyapatite spacers, with the tumor located on the side of the LP. Cervical spine alignment was maintained at the final follow-up of 6 years in both cases. | LP 0/2 | NA |
| Kobayashi et al. [21] (2018) | Retrospective cohort study | Mean age: conical LP (45.3 yr), T-saw LP (48.6 yr), LE (53.8 yr); conical LP (n=21), T-saw LP (n=17), LE (n=16); M (n=30), F (n=24) | Ependymoma; schwannoma; hemangioma; meningioma; hemangioblastoma; astrocytoma; neurofibroma; others | Conical LP (the bone graft fixing by sutures); T-saw LP (posterior arches are reconstructed with sutures); thoracic | 41 | Association recovery rates did not differ significantly among the three groups. Sagittal kyphosis significantly worsened at final follow-up in LE group, but did not change significantly in LP groups. | Not reported | ***/**/*** |
| Shirosaka et al. [22] (2018) | Retrospective case series | Mean age: 41.6 yr; n=14; M (n=8), F (n=6) | Anaplastic ependymoma; hemangioblastoma; germ cell tumor; ependymoma; cavernoma; schwannoma; meningioma; subependymoma | Lift-up LP with titanium basket plates; cervical | 17.2 | In the 14 patients, a total of 32 cervical laminae were reconstructed after resection of intradural tumors. Mean operation time including resection of the tumor was 473 min (range, 250ŌĆō637 min). Mean estimated blood loss including the resection of the tumor was 261 mL (range, 40ŌĆō700 mL). Imaging analysis demonstrated no significant change in C2ŌĆōC7 angle cervical range of motion between before and after surgery, suggesting sequential spinal stability at the base of the laminae. | None | NA |
| Emel et al. [23] (2017) | Retrospective cohort study | Mean age: 45.8 yr; LP (n=19), LE (n=23), HLE (n=7); M (n=21), F (n=26) | Schwannoma | LP with bilaterally sutured laminae using a strong non-absorbable suture; cervical, thoracic, lumbar, sacral | 61.4 | LP was better than hemi-LE and LE approaches in the length of stay with averages of 2.9┬▒1.05 days, versus 5┬▒2.16 days, and 9.5┬▒7.17 days, respectively. The mean intraoperative blood loss was less in LP with an average of 395 mL and in hemi-LE with average of 435 mL versus an average of 1,130 mL in cases who underwent LE. | LP 1/19; LE 2/23; HLE 1/7 | **/*/*** |
| Siller et al. [24] (2016) | Retrospective case series | Mean age: 36.8 yr; LP (n=6), LE (n=15), HLE (n=5); M (n=12), F (n=12) | Hemangioblastoma | Not reported; cervical, thoracic, lumbar | 94.8 | No surgical approach-related outcomes reported. | Not divided into groups: 5/24 | NA |
| Montano et al. [25] (2014) | Retrospective cohort study | Mean age: 51.07 yr; LP (n=24), LE (n=19); M (n=18), F (n=25) | Schwannoma; cavernoma; ependymoma; meningioma; hemangioblastoma; low-grade astrocytoma; metastasis; fibrous tumor | LP with titanium microplates; cervical, thoracic, lumbar | 24.41 | Nine patients developed deformity or experienced a worsening of preoperative deformity at latest follow-up. Among the considered potential prognostic factors, LE (p=0.03) and evidence of pre-operative spinal deformity (p=0.009) were significantly associated with new-onset or worsening of spinal deformity. With logistic regression analysis, only the performed surgical procedure emerged as an independent prognostic factor (p=0.044). Mean hospital stay was 7.73┬▒2.53 days in the LE and 6.62┬▒1.83 days in the LP. Mean operation length was 171.57┬▒41.66 min in the LE and 175.41┬▒36.47 min in the LP. | LP 0/24; LE 2/19 | ****/**/*** |
| Parker et al. [26] (2013) | Retrospective case series | Mean age: 38.0 yr; LP (n=40); M (n=20), F (n=20) | Ganglioglioma; dermoid; ependymoma; arachnoid cyst; germ-cell tumor; lipoma; cavernous malformation; pilocytic astrocytoma; gliosis; exophytic solitary fibrous tumor; paraganglioma; schwannoma; meningioma; arteriovenous; malformation; neuropathic pain syndrome; dermal sinus tract resection and cord; untethering; myxopapillary; ependymoma; neuroenteric cyst; hemangioblastoma; intradural lipoma and tethered cord release; low-grade glioma; neurofibroma | LP with Leibinger titanium fixation plates; cervical, thoracic, lumbar | 6.4 | Successful LP was carried out in all 40 patients. Median (interquartile range) intraoperative blood loss in this series was 150 mL (75ŌĆō300 mL). | LP 2/40 | NA |
| Zhou et al. [27] (2013) | Retrospective case series | Mean age: 40.7 yr; LP (n=13); M (n=5), F (n=8) | Neurilemmoma; hemangioma; meningioma; ependymoma; astrocytoma | LP with arch plate fixation; thoracic, lumbar | 9ŌĆō22 | The VAS and ODI results 2 weeks following surgery and at the final follow-up examination demonstrated a significant improvement compared with the corresponding preoperative results. Radiographs demonstrated satisfactory positioning of instrumentation without any evidence of fracture, lumbar scoliosis, kyphosis, or instability. | LP 1/13 | NA |
| Menku et al. [28] (2010) | Prospective case series | Mean age: 42.3 yr; LP (n=45); M (n=25), F (n=20) | Astrocytoma; ependymoma; dermoid; lipoma; neurinoma; meningioma; cavernous angioma; syringomelia | LP with laminar flap and fixation with mini-plates; thoracic, lumbar | 12 | No patients had kyphosis and/or instability on static or dynamic plain X-ray films done at 3, 6, and 12 months. There were no cases of dural, nerve root, or spinal cord injuries attributable to laminotomy or laminar flap replacement. Bony healing was confirmed radiologically in 91% of the laminae. There was no scar tissue invasion in the spinal canal based on the MRI findings. | None | NA |
| McGirt et al. [29] (2010) | Retrospective cohort study | Mean age: 46 yr; LP (n=58), LE (n=180); M (n=108), F (130) | Ependymoma; low-grade astrocytoma; hemangioblastoma; ganglioglioma; malignant astrocytoma; metastasis; cavernoma; medulloblastoma; schwannoma; meningioma; lipoma; neurofibroma; dermoid | LP with titanium microplates; cervical, thoracic, lumbar | 24 | All baseline clinical, radiographic, and operative variables were similar between the LP and LE cohorts. LP was associated with a decreased mean length of hospitalization (5 days vs. 7 days; p=0.002) and trend of decreased incisional CSF leak (3% vs. 9%; p=0.14). Following LP vs. LE, 5 (9%) vs. 21 (12%) patients developed progressive deformity (p=0.728) a mean of 14 months after surgery. The incidence of progressive deformity was also similar between LP vs. LE in pediatric patients <18 years of age (43% vs. 36%), with preoperative scoliosis or loss of cervical/lumbar lordosis (28% vs. 22%), or with intramedullary tumors (11% vs. 11%). | LP 9/58; LE 25/180 | ***/**/*** |
| Iplikcioglu et al. [30] (2010) | Retrospective case series | Mean age: 44.3 yr; LP (n=17); M (n=8), F (n=9) | Astrocytoma; meningiomas; neurinomas; ependymomas; EwingŌĆÖs sarcoma, metastasis; abscess; hemangioblastoma; arachnoid cyst; lipoma | Open-door LP with silk sutures or titanium miniplates with screws; cervical, thoracic, lumbar | 30 | All lesions were exposed using the open-door LP technique and were successfully removed for intraspinal mass lesions. An average of 3.7 level LP was performed. Neither spinal malalignment on the coronal plane nor displacement of bone flap (LP flap) were observed on postoperative CT and MR examinations. | LP 1/17 | NA |
| Liu et al. [31] (2009) | Retrospective case series | Mean age: 36.2 yr; LP (n=24); M (n=15), F (n=9) | Neurofibroma; ependymoma; lipoma; teratoma | LP with silk or nylon sutures; thoracic, lumbar | 34.2 | Sixty-six laminae were re-implanted in 24 patients. The average operative time was 137 min (range 90ŌĆō205 min). Mean blood loss was 320 mL (260ŌĆō600 mL). According to postoperative X-rays, MRI, and/or CT, fusion of laminae was achieved in 3 to 6 months (mean, 4.5 months). The preoperative and postoperative Cobb angles were 16.5┬░┬▒5.0┬░ and 18.4┬░┬▒11.4┬░, respectively, and there was no significant difference (p>0.05). Unilateral healing of the incision lines was observed in seven cases, including one with two-level laminotomy, three with three-level laminotomy, and three with four-level laminotomy. The other 17 cases underwent bilateral fusion. | LP 2/24 | NA |
| Sciubba et al. [32] (2008) | Retrospective case series | Mean age: 41 yr; LP (n=6), LE (n=26); M (n=16), F (n=16) | Astrocytoma; ependymoma; hemangioblastoma; ganglioglioma; schwannoma; subependymoma; chordoma; meningioma; neurofibroma; intradural metastatic lesions; leiomyoma; cyst | Not reported; cervical | 25.2 | Each additional level of LE performed was associated with a 3.1-fold increase in the likelihood of subsequent vertebral instability (odds ratio, 3.114; 95% confidence interval, 1.207ŌĆō8.034; p=0.02). 33% (4 of 12) of the patients who had undergone a Ōēź3-level LE required subsequent fusion compared with 5% (1 of 20) who had undergone a Ōēż2-level LE (p=0.03). Four (36%) of 11 patients initially presenting with myelopathic motor disturbance required subsequent fusion compared with 1 (5%) of 21 presenting initially with myelopathic sensory or radicular symptoms (p=0.02). Age, the presence of a syrinx, intramedullary tumor, C-2 LE, C-7 LE, and LP were not associated with subsequent symptomatic instability requiring fusion. | Not divided into groups: 5/32 | NA |
| Hida et al. [33] (2006) | Retrospective case series | Mean age: 60.1 yr; LP (n=8); M (n=5), F (n=3) | Neurilemoma; hemangioma; ossification of yellow ligament; spontaneous spinal cord herniation | Transverse placement LP with titanium miniplates; thoracic, lumbar | 24 | Mean blood loss was 219 g (range, 45ŌĆō600 g), and the mean duration of surgery was 3 hr 54 min (range, 2 hr 50 minŌĆō6 hr 20 min). Bony fusion of reconstructed laminae was noted at a mean of 3.2 months. No cases of spinal deformity, epidural hematoma, scar tissue in the spinal canal, or back pain were noted. | Not reported | NA |
| Casha et al. [34] (2004) | Retrospective case series | Mean age: 57 yr; LP: tumor case (n=9), non-tumor case (n=19); M (n=18), F (n=10) | Ependymoma; astrocytoma; sarcoidosis; metastatic carcinoma; schwannoma | En bloc LP with titanium miniplates; cervical | 15 | The mean angular extensionŌĆōflexion displacement measured between C1 and C7 was unchanged postoperatively, with preserved mobility across LP-treated segments in all patients. The anteroposterior diameter of the spinal canal increased 3.6 mm (27.2%) postoperatively (p=0.004). In one patient an asymptomatic postoperative kyphosis developed. | 5/28 | NA |
| Asazuma et al. [35] (2004) | Retrospective cohort study | Mean age: 49.0 yr; LP (n=22), LE (n=14), HLE (n=15); M (n=25), F (n=26) | Neurinoma; meningioma; ependymoma; neurofibroma | Expansive open-door LP; cervical | 52 | Worsening of cervical curvature type was statistically less frequent with hemi-LE than LP or LE (p<0.05), although no significant difference was evident overall between pre- and postoperative cervical curvature indices or ROM in any group. Cases of C2 surgery had more frequent curvature worsening (80%) in the LP group than in other groups (p<0.05). Postoperative changes of the cervical curvature in patients with cervical spinal cord tumors were greatly influenced by the surgical method; the cervical curvature was particularly unfavorable when patients had C2 decompression. | Not reported | */*/** |
| Asazuma et al. [36] (2003) | Retrospective case series | Mean age: 55.7 yr; LP (n=7); M (n=1), F (n=6) | Neurinoma; meningioma; neurofibroma | 90┬░ rotational LP; thoracic, lumbar | 29 | The tumor was totally removed in all cases. The JOA score improved from 62.5% to 100% (average: 81.9%). The change in the postoperative intervertebral range of motion was a 5.0┬░ decrease to a 5.0┬░ increase (average: 0.4┬░ decrease). The change in lordosis varied from a 9┬░ decrease to a 11┬░ increase (average: 1.3┬░ increase). Bony union was confirmed and the rotated laminae remained in situ in all seven cases. | Not reported | NA |
| Kawahara et al. [37] (1999) | Prospective case series | Mean age: 46.1 yr; LP (n=24); M (n=14), F (n=10) | Neurinoma; ependymoma; hemangioma; epidermoid cyst; meningioma | T-saw LP; thoracic, lumbar | 47 | Primary bony union in 23 patients by 6 months after surgery, and in one patient by 12 months after surgery. No complications such as postoperative spinal canal stenosis, facet arthrosis, or kyphosis were observed. | None | NA |
| Inoue et al. [38] (1996) | Retrospective cohort study | Mean age: 42.5 yr; LP (n=10), LE (n=18), HLE (n=7); M (n=22), F (n=14) | Astrocytoma; neurinoma; ganglio-neurinoma; neurofibroma; ependymoma; meningioma; lipoma; syringomyelia; cavitation of spinal cord; enterogenous cyst | Not reported; cervical | 48 | In the LE group, kyphosis of the upper cervical spine and compensatory increased lordosis of the lower cervical spine were observed in the C2 LE patients. Localized kyphosis of the spine at the cervicothoracic junction and compensatory increased lordosis of the upper cervical vertebrae were noted in the C7 LE patients. In the LP group, spinal deformities were less frequently observed, and when present, the deformity was limited to a slight increase of lordosis, even in patients who had the facetectomy. | Not reported | **/**/*** |
LP, laminoplasty; LE, laminectomy; HLE, hemilaminectomy; M, male; F, female; CSF, cerebrospinal fluid; ASIA, American Spinal Cord Injury Association; NA, not applicable; ODI, Oswestry Disability Index; VAS, Visual analog Scale; MRI, magnetic resonance imaging; CT, computed tomography; MR, magnetic resonance; ROM, range of motion; JOA, Japanese Orthopaedic Association.
References
1. Arnautovic KI, Gokaslan ZL. Spinal cord tumors. Cham: Springer International Publishing; 2019.
2. Munns J, Park DK, Deutsch H, Singh K. Primary spinal cord tumors: Part I-extradural and extramedullary tumors. Contemp Spine Surg 2009;10:1ŌĆō8.
3. Schellinger KA, Propp JM, Villano JL, McCarthy BJ. Descriptive epidemiology of primary spinal cord tumors. J Neurooncol 2008;87:173ŌĆō9.



4. Shao MM, Rubino S, DiRisio DJ, German JW. The history of neurosurgical spinal oncology: from inception to modern-day practices. World Neurosurg 2021;150:101ŌĆō9.


5. Hirano Y, Ohara Y, Mizuno J, Itoh Y. History and evolution of laminoplasty. Neurosurg Clin N Am 2018;29:107ŌĆō13.


6. Raimondi AJ, Gutierrez FA, Di Rocco C. Laminotomy and total reconstruction of the posterior spinal arch for spinal canal surgery in childhood. J Neurosurg 1976;45:555ŌĆō60.


7. Papagelopoulos PJ, Peterson HA, Ebersold MJ, Emmanuel PR, Choudhury SN, Quast LM. Spinal column deformity and instability after lumbar or thoracolumbar laminectomy for intraspinal tumors in children and young adults. Spine (Phila Pa 1976) 1997;22:442ŌĆō51.


8. Phan K, Scherman DB, Xu J, Leung V, Virk S, Mobbs RJ. Laminectomy and fusion vs laminoplasty for multi-level cervical myelopathy: a systematic review and meta-analysis. Eur Spine J 2017;26:94ŌĆō103.



9. Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Int J Surg 2021;88:105906.


10. Shea BJ, Reeves BC, Wells G, et al. AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ 2017;358:j4008.



11. Amir-Behghadami M, Janati A. Population, Intervention, Comparison, Outcomes and Study (PICOS) design as a framework to formulate eligibility criteria in systematic reviews. Emerg Med J 2020;37:387.


13. Wells GA, Shea B, OŌĆÖConnell D, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Ottawa (ON): Ottawa Hospital Research Institute; 2000.
14. Hao X, Lin W. Vertebral plate and ligament composite laminoplasty in spinal cord tumor surgery: analysis of 94 patients. Transl Neurosci 2021;12:40ŌĆō5.



15. Tatter C, Fletcher-Sandersjoo A, Persson O, et al. Incidence and predictors of kyphotic deformity following resection of cervical intradural tumors in adults: a population-based cohort study. Acta Neurochir (Wien) 2020;162:2905ŌĆō13.




16. Kumar R, Debbarma I, Boruah T, et al. Flipped reposition laminoplasty for excision of intradural extramedullary tumors in the thoracolumbar spine: a case series of 14 patients. Asian Spine J 2020;14:327ŌĆō35.




17. Cofano F, Giambra C, Costa P, et al. Management of extramedullary intradural spinal tumors: the impact of clinical status, intraoperative neurophysiological monitoring and surgical approach on outcomes in a 12-year double-center experience. Front Neurol 2020;11:598619.



18. Song Z, Zhang Z, Ye Y, Zheng J, Wang F. Efficacy analysis of two surgical treatments for thoracic and lumbar intraspinal tumours. BMC Surg 2019;19:131.




19. Onyia CU, Menon SK. Laminectomy versus laminoplasty in the surgical management of long-segment intradural spinal tumors: any difference in neurological outcomes? Asian J Neurosurg 2018;13:1128ŌĆō33.



20. Miyakoshi N, Kudo D, Hongo M, Kasukawa Y, Ishikawa Y, Shimada Y. Intradural extramedullary tumor in the stenotic cervical spine resected through open-door laminoplasty with hydroxyapatite spacers: report of two cases. BMC Surg 2018;18:38.




21. Kobayashi K, Imagama S, Ando K, Nishida Y, Ishiguro N. Efficacy of conical laminoplasty after thoracic laminectomy. Clin Spine Surg 2018;31:156ŌĆō61.


22. Shirosaka K, Naito K, Yamagata T, Yoshimura M, Ohata K, Takami T. Cervical lift-up laminoplasty with titanium basket plates after resection of intradural tumor. J Craniovertebr Junction Spine 2018;9:26ŌĆō31.



23. Emel E, Abdallah A, Sofuoglu OE, et al. Long-term surgical outcomes of spinal schwannomas: retrospective analysis of 49 consecutive cases. Turk Neurosurg 2017;27:217ŌĆō25.

24. Siller S, Szelenyi A, Herlitz L, Tonn JC, Zausinger S. Spinal cord hemangioblastomas: significance of intraoperative neurophysiological monitoring for resection and long-term outcome. J Neurosurg Spine 2017;26:483ŌĆō93.


25. Montano N, Trevisi G, Cioni B, et al. The role of laminoplasty in preventing spinal deformity in adult patients submitted to resection of an intradural spinal tumor: case series and literature review. Clin Neurol Neurosurg 2014;125:69ŌĆō74.


26. Parker SL, Kretzer RM, Recinos PF, et al. Ultrasonic BoneScalpel for osteoplastic laminoplasty in the resection of intradural spinal pathology: case series and technical note. Neurosurgery 2013;73(1 Suppl Operative): ons61ŌĆō6.

27. Zhou D, Nong LM, Gao GM, Jiang YQ, Xu NW. Application of lamina replantation with ARCH plate fixation in thoracic and lumbar intraspinal tumors. Exp Ther Med 2013;6:596ŌĆō600.



28. Menku A, Koc RK, Oktem IS, Tucer B, Kurtsoy A. Laminoplasty with miniplates for posterior approach in thoracic and lumbar intraspinal surgery. Turk Neurosurg 2010;20:27ŌĆō32.

29. McGirt MJ, Garces-Ambrossi GL, Parker SL, et al. Short-term progressive spinal deformity following laminoplasty versus laminectomy for resection of intradural spinal tumors: analysis of 238 patients. Neurosurgery 2010;66:1005ŌĆō12.

30. Iplikcioglu AC, Hatiboglu MA, Ozek E, Dinc C, Erdal M. Surgical removal of spinal mass lesions with open door laminoplasty. Cent Eur Neurosurg 2010;71:213ŌĆō8.


31. Liu XY, Zheng YP, Li JM. Laminoplasty for the treatment of extramedullary intradural tumors in the thoracic and lumbar spine: greater than two-year follow-up. Orthop Surg 2009;1:275ŌĆō9.



32. Sciubba DM, Chaichana KL, Woodworth GF, McGirt MJ, Gokaslan ZL, Jallo GI. Factors associated with cervical instability requiring fusion after cervical laminectomy for intradural tumor resection. J Neurosurg Spine 2008;8:413ŌĆō9.


33. Hida S, Naito M, Arimizu J, Morishita Y, Nakamura A. The transverse placement laminoplasty using titanium miniplates for the reconstruction of the laminae in thoracic and lumbar lesion. Eur Spine J 2006;15:1292ŌĆō7.




34. Casha S, Engelbrecht HA, DuPlessis SJ, Hurlbert RJ. Suspended laminoplasty for wide posterior cervical decompression and intradural access: results, advantages, and complications. J Neurosurg Spine 2004;1:80ŌĆō6.


35. Asazuma T, Nakamura M, Matsumoto M, Chibo K, Toyama Y. Postoperative changes of spinal curvature and range of motion in adult patients with cervical spinal cord tumors: analysis of 51 cases and review of the literature. J Spinal Disord Tech 2004;17:178ŌĆō82.

36. Asazuma T, Yamagishi M, Sato M, Ichimura S, Fujikawa K. Vertebral arch reconstruction based on 90 degree rotational laminoplasty after removal of spinal cord and cauda equina tumours. Acta Neurochir (Wien) 2003;145:495ŌĆō500.



37. Kawahara N, Tomita K, Shinya Y, et al. Recapping T-saw laminoplasty for spinal cord tumors. Spine (Phila Pa 1976) 1999;24:1363ŌĆō70.


38. Inoue A, Ikata T, Katoh S. Spinal deformity following surgery for spinal cord tumors and tumorous lesions: analysis based on an assessment of the spinal functional curve. Spinal Cord 1996;34:536ŌĆō42.



39. Ruspi ML, Chehrassan M, Faldini C, Cristofolini L. In vitro experimental studies and numerical modeling to investigate the biomechanical effects of surgical interventions on the spine. Crit Rev Biomed Eng 2019;47:295ŌĆō322.


40. Healy AT, Lubelski D, West JL, Mageswaran P, Colbrunn R, Mroz TE. Biomechanics of open-door laminoplasty with and without preservation of posterior structures. J Neurosurg Spine 2016;24:746ŌĆō51.


41. Subramaniam V, Chamberlain RH, Theodore N, et al. Biomechanical effects of laminoplasty versus laminectomy: stenosis and stability. Spine (Phila Pa 1976) 2009;34:E573ŌĆō8.

42. Wang DL, Zhu GQ, Huang AQ, et al. The anatomical and biomechanical superiority of novel posterior en bloc elevation cervical laminoplasty. Surg Innov 2021;28:552ŌĆō9.



43. Tejapongvorachai T, Tanaviriyachai T, Daniel Riew K, et al. Curved versus straight-cut hinges for open-door laminoplasty: a finite element and biomechanical study. J Clin Neurosci 2020;78:371ŌĆō5.


44. Sun S, Li Y, Wang X, et al. Safety and efficacy of laminoplasty versus laminectomy in the treatment of spinal cord tumors: a systematic review and meta-analysis. World Neurosurg 2019;125:136ŌĆō45.


45. Raab P, Juergen K, Gloger H, Soerensen N, Wild A. Spinal deformity after multilevel osteoplastic laminotomy. Int Orthop 2008;32:355ŌĆō9.











