Introduction
Pedicle screw fixation of the cervical spine has become a popular alternative to lateral mass screw fixation because of its higher anchorage strength. This technique provides excellent fixation. However, it carries a latent risk of injury to the spinal cord, nerve roots, and vertebral arteries. Identifying an accurate entry point for the pedicle screw is a critical step for preventing these unfavorable events, but this is difficult because of the small number of landmarks due to anatomical features of the cervical spine, such as the flattened shape of the cervical laminae.
To improve the accuracy of pedicle screw placement, several methods have been advocated, including an intraoperative navigation system [1], an intraoperative pedicle axis view technique using fluoroscopy [2], and the computed tomography (CT) cutout technique [3]. These techniques enable safer and more accurate pedicle screw placement in the cervical spine compared with the free-hand technique, but they cannot fully eliminate the risk of screw misplacement.
Several studies have evaluated the three-dimensional morphology of the cervical pedicle to identify an accurate insertion point for the pedicle screw [45678]. Most studies have employed the lateral mass, lateral vertical notch, and/or inferior articular process as landmarks to identify an insertion point for the pedicle screw. However, we often encounter patients in whom we cannot identify an accurate insertion point for the pedicle screw using these landmarks. Degenerative changes in the facet joints, which are frequently observed in patients who are indicated for posterior cervical fixation, significantly affect the morphology of these landmarks. We need a better landmark to identify the insertion points for pedicle screws regardless of the presence of degenerative changes.
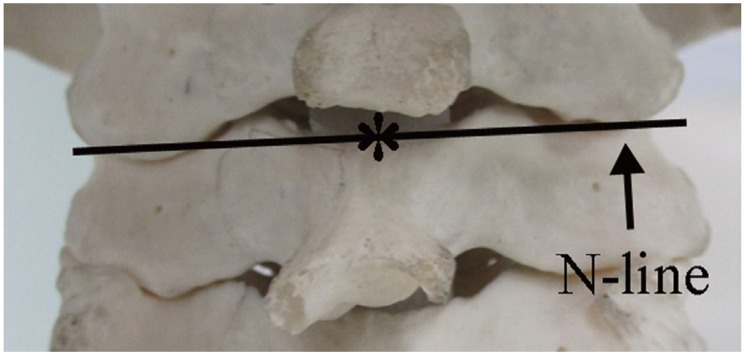
The superomedial edge of the lamina (asterisk in Fig. 1) is less affected by degenerative changes. We hypothesized that it could be a new landmark for identifying an accurate cervical insertion point for the pedicle screw. In this study, the line passing through the superomedial edge of the lamina and intersecting the base of the spinous process at a right angle was termed the “N-line” (novel line) (Fig. 1). In the present study, we used neck CT images to evaluate the suitability of the superomedial edge of the lamina, i.e., the N-line, as a landmark for identifying an accurate insertion point for the cervical pedicle screw.
Materials and Methods
1. Participants
The participants in this study were patients who underwent neck CT scanning for the determination of neck disease in our institute from April to October 2012. A total of 327 consecutive patients were recruited for the analysis. There were 96 women and 231 men, with a mean age of 60.3 years (range, 18–87 years). Patients with fine-quality images of the third through the seventh cervical vertebrae who were aged 18 years or over at the time of imaging were included in the study. Patients with previous cervical spine surgery, neoplasms, trauma, or congenital anomalies were excluded. We evaluated 1,635 cervical vertebrae in 327 patients.
This study was approved by an Institutional Review Board (No. 24-123).
2. Radiological examination
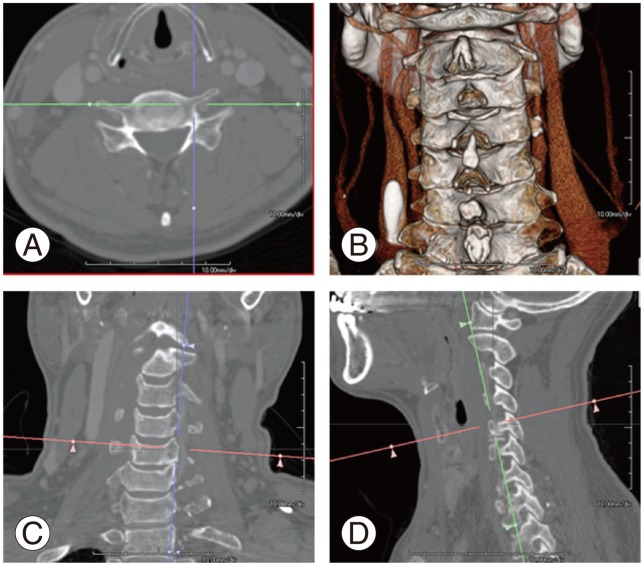
All neck CT scans were axial, 1.0-mm thick, sequential, and obtained with the patient in the supine position without gantry tilt (120 kV, 160 mA, 0.5 seconds) using a Toshiba Aquilion CX (Toshiba Medical Systems Corporation, Tokyo, Japan). These data were reconstructed in the condition suitable for bone evaluation by a software application (AquariusNet Viewer, TeraRecon, CA, USA). This software application allows us to reconstruct optional sagittal (Fig. 2D), coronal (Fig. 2C), and axial (Fig. 2A), and 3D (Fig. 2B) views to evaluate the morphology of the cervical spine.
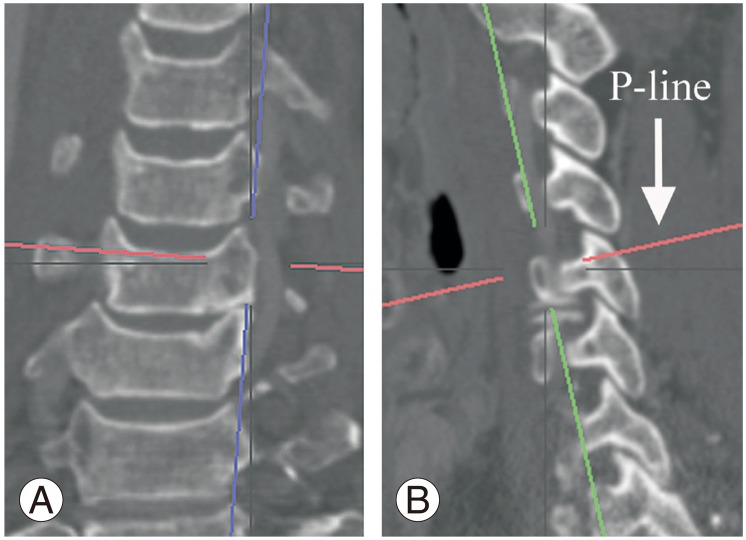
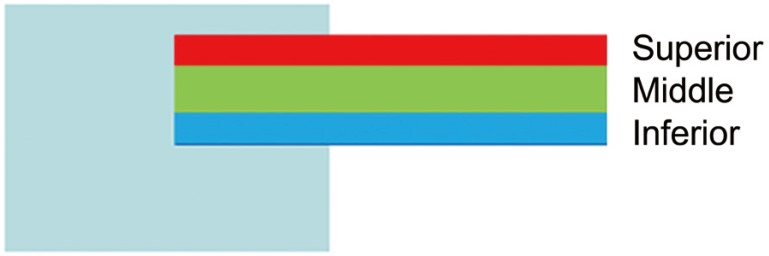
At first, the line was drawn parallel to the superior border of the pedicle in the sagittal plane, which was termed the “P-line” (pedicle line) (Fig. 3B), and parallel to the vertical body in the coronal plane (Fig. 3A). The P-line was moved downward in 1-mm increments to the inferior border of the pedicle (Fig. 4). The P-line passing through the superomedial edge of the lamina was termed the “N2-line” (Fig. 5B). The N-line and the N2-line lie in the same plane. We then evaluated whether the N2-line (N-line) was located between the superior and inferior borders of the pedicle in the sagittal plane (Fig. 5). We also divided the pedicle into superior, middle, and inferior parts (Fig. 6).
Results
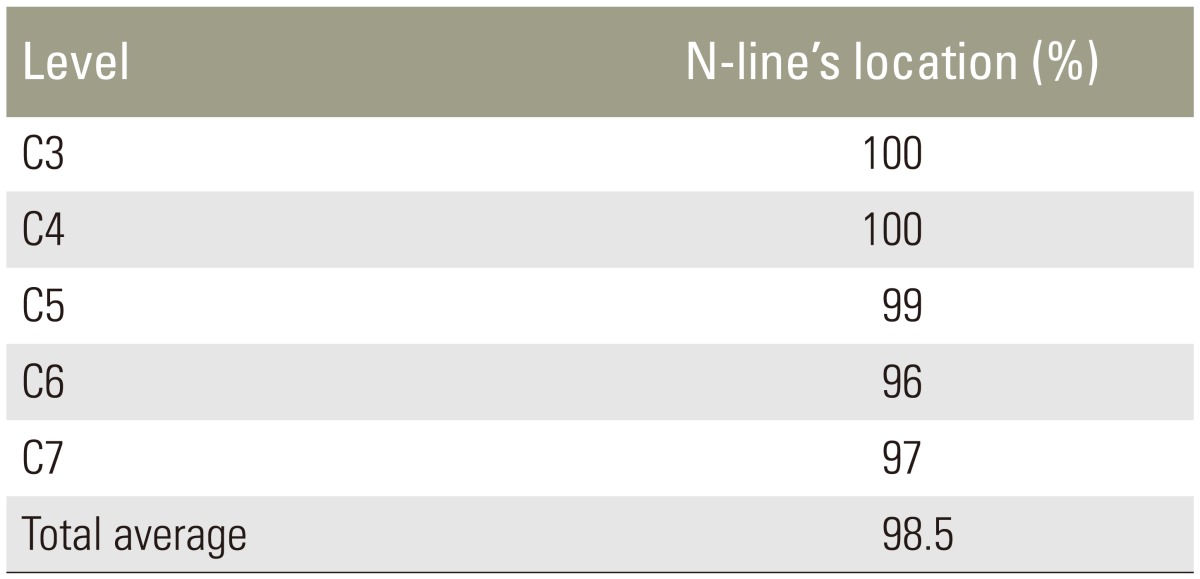
The percentages of N-lines located between the superior and inferior borders of the pedicle were 100% at C3, 100% at C4, 99% at C5, 96% at C6, and 97% at C7 (Table 1). In total, 98.5% of the N-lines were located between the superior and inferior borders of the pedicle.
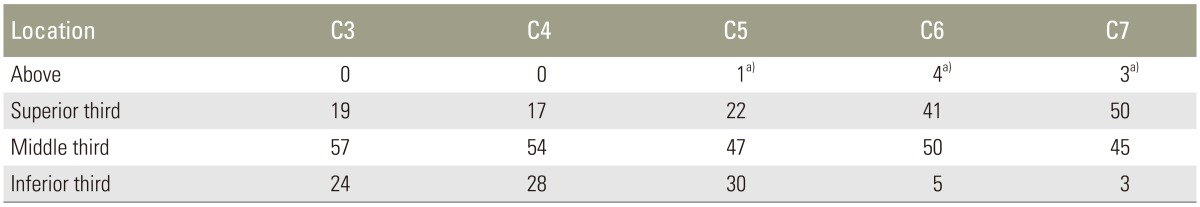
We determined through which of the three regions of the pedicle (superior, middle, or inferior) the N-lines passed. Nineteen percent of the N-lines at C3 were located in the superior third of the pedicle, 57% were in the middle third, and 24% were in the inferior third. Seventeen percent of the N-lines at C4 were located in the superior third of the pedicle, 54% were in the middle third, and 28% were in the inferior third. Twenty-two percent of the N-lines at C5 were located in the superior third of the pedicle, 47% were in the middle third, and 30% were in the inferior third. One percent of the N-lines at C5 were located above the level of the superior border of the pedicle; all were located within 1 mm of the border. Forty-one percent of the N-lines at C6 were located in the superior third of the pedicle, 50% were in the middle third, and 5% were in the inferior third. Four percent of the N-lines at C6 were located above the level of the superior border of the pedicle; all were located within 1 mm of the border. Fifty percent of the N-lines at C7 were located in the superior third of the pedicle, 45% were in the middle third, and 3% were in the inferior third. Three percent of the N-lines at C7 were located above the level of the superior border of the pedicle; all were located within 1 mm of the border (Table 2). The most frequent location of the N-line was the lower cervical spine. One percent of the N-lines at C5, 4% of the N-lines at C6, and 3% of the N-lines at C7 were located above the level of the superior border of the pedicle; all were located within 1 mm of the border. There were no significant differences between men and women or in members of different age groups in the location of the N-line.
Discussion
After Abumi and Kaneda [9] advocated pedicle screw fixation for the middle and lower cervical spine, this procedure has become a popular alternative method to other posterior cervical fixation procedures because of its higher anchorage strength. Biomechanical studies have shown that cervical pedicle screw fixation provides enhanced screw purchase compared with other posterior cervical fixation procedures [101112]; however, this technique carries a latent risk of injury to the spinal cord, nerve roots, and vertebral arteries [131415]. Several methods have been advocated to insert cervical pedicle screws safely and accurately.
Yukawa et al. [2] achieved good clinical results in patients with unstable cervical injury by inserting cervical pedicle screws with the use of a fluoroscopy-assisted pedicle axis view technique. Miyamoto and Uno [3] inserted pedicle screws using the CT cutout technique. In this technique, the preoperative CT image is developed at life-size on film and cut out according to the lamina surface. The film is sterilized and used as an intraoperative guide when the pedicle screws are inserted. The authors reported that this technique is an easy and low-cost procedure, which provides safe insertion of the pedicle screw in the cervical spine. Rahmathulla et al. [1] reported that the combination of 3D imaging with intraoperative navigation systems improves the accuracy and safety of pedicle screw placement, especially in patients with complex spinal deformities.
These techniques enable cervical pedicle screws to be inserted safely and more accurately with lower latent risks; however, they cannot fully promise successful placement of cervical pedicle screws. It is therefore very important to understand the morphology of the cervical spine. Several studies have evaluated the 3D morphology of the cervical pedicle to determine the insertion point for pedicle screws.
Karaikovic et al. [4] investigated the landmarks for the insertion point of cervical pedicle screws using normal cervical spines of human cadavers, and found that the lateral vertebral notch and the inferior articular processes were landmarks for C3–7. Rao et al. [5] provided normative data on subaxial cervical pedicle geometry from CT scans in a large number of young, healthy volunteers. Lee et al. [6] tried to determine the optimal insertion points and trajectories for cervical pedicle screw insertion using 3D CT images. They proposed three topographic bony landmarks: the lateral vertebral notch, the center of the superior ridge of the lateral mass, and the center of the lateral mass.
Is there any landmark for the placement of cervical pedicle screws that is not affected by degenerative changes of the cervical spine? We focused on the superomedial edge of the lamina, which is less affected by degenerative change because it does not construct the joint anatomically. In addition, it is not difficult to find during surgery. We hypothesized that this point could be a new landmark for the insertion point of the cervical pedicle screw.
In this study, we found that the N-line was frequently located at the level of the pedicle of each cervical spine in the sagittal plane. In C3 and C4, 100% of the N-lines were in this location. In a few cases, the N-line at the C5, C6, or C7 level was located above the superior border of the pedicle, but it was always within 1 mm of the border. We also found that the N-line tends to have a cranial location in the lower cervical spine. All of these findings suggest that the N-line is a useful reference to determine the accurate insertion point of the cervical pedicle screw in the sagittal plane.
The insertion angle and the entry points for pedicle screws govern the accuracy of cervical pedicle screw placement. The insertion angle is different in each patient, as the morphology of the pedicle is peculiar to each individual; however, we can estimate the insertion angle during surgery based on preoperative CT images.
It is often difficult to identify accurate entry points for pedicle screws because of degenerative changes, especially around the area of the facet joints, which are frequently observed in patients who are indicated for posterior cervical fixation. The N-line passes through the superomedial edge of the lamina and intersects the base of the spinous process at a right angle (Fig. 1). We can determine the N-line during surgery regardless of any degenerative changes in the cervical spine, since the edge is less involved in degenerative changes. In the present study, we clearly showed that the N-line can be a new landmark to determine the entry point for pedicle screws in the sagittal plane.
Of course, it is not so easy to draw a line accurately intersecting the base of the spinous process at a right angle in the operative field. In addition, we cannot determine accurate entry points for pedicle screws using the N-line alone, since it cannot be a landmark for the entry points of pedicle screws in the axial plane. We realize that an error of only 1 mm could be critical in deciding the insertion point of a cervical pedicle screw and consider it is important to use other methods, including fluoroscopy and so on. However, we believe that the fact the superomedial edge of the lamina is frequently located at the level of the pedicle on each cervical spine is helpful for pedicle screw insertion.
A limitation of this study is that the capability of the N-line as a landmark to determine the entry point for pedicle screws was evaluated on CT images, not in clinical practice. A prospective study is ongoing to evaluate the capability of the N-line in clinical practice.
Conclusions
We found that the N-line was frequently located at the level of the pedicle of each cervical spine in the sagittal plane. We consider that the superomedial edge of the lamina could be a new landmark for the insertion point of cervical pedicle screws and would enable safer and more accurate placement of the screws.