 |
 |
- Search
| Asian Spine J > Volume 13(3); 2019 > Article |
|
Abstract
Purpose
To evaluate the efficacy of Schroth therapy on thoracic curve angle, pain, and self-perceived body image (SPBI) of the back in Scheuermann’s patients in comparison with the efficacy of classic anti-gravitation exercises.
Overview of Literature
Scheuermann disease is the most common cause of hyperkyphosis of the thoracic and thoracolumbar spine during adolescence. However, very few studies evaluated the effect of exercises on the progression of kyphosis in Scheuermann patients. Schroth three-dimensional exercise therapy was found in several studies to be effective in the treatment of adolescent scoliosis; however, we found no randomized controlled trials that evaluated the efficacy of this method in Scheuermann patients.
Methods
A total of 50 young adults (males and females) with Scheuermann’s disease were randomly divided into either the experimental group (Schroth therapy treatment, n=25) or the control group (classic anti-gravitation exercises, n=25). Participants in both the groups were provided a course of individual treatment sessions during few weeks, with one appointment per week. They were required to perform the exercises daily throughout the study period (12 months) and fill their performance in a research log. We evaluated the thoracic Cobb angle (main outcome measure), pain, SPBI, flexion of the shoulder (supine), flexion of the shoulder (standing), kyphotic deformity measured using inclinometer, and L5 kyphosis apex line (L5-KAL) as well as administered the Scoliosis Research Society-22 Questionnaire for the participants before the treatment, after 6 months, and 1 year postoperatively. These results were then compared.
Results
In the mixed analysis of variance, the main effect of time was significant in the thoracic kyphosis (F [1]=5.72, p=0.02), and in the L5-KAL (F [1]=5.76, p=0.02). The main effect of time on the kyphotic deformity, measured using an inclinometer, did not reach the significance level; however, it showed the tendency (F [1]=2.80, p=0.07). In the group-by-time interaction, a significant difference was found in the thoracic kyphosis (F [1]=4.91, p=0.03) and in the kyphotic deformity, measured using an inclinometer (F [1]=4.05, p=0.02). Thus, the Schroth therapy group showed significantly greater improvement than the classic anti-gravitation exercises group.
Scheuermann’s disease is the most common cause of hyperkyphosis of the thoracic and thoracolumbar spine during adolescence period. It is the most common disorder after idiopathic scoliosis in patients with spine deformities [1,2]. Most commonly, the patient is aged 12–15 years of age [3,4].
One of the early clinical signs of Scheuermann’s disease is anterior rounded shoulders and occasionally anterior flexion contractures of the shoulder joint, which lead to limited pure shoulder flexion. Moreover, patients with Scheuermann’s disease have an angular thoracic kyphosis, often with compensatory lumbar lordosis and increased cervical lordosis. The deformity is relatively fixed and cannot be flattened while hyperextension of the back [1,3,4]. Pain, when present, usually is mild and induced by prolonged periods of sitting or exercise, usually being located near the apex of the deformity. In most cases, the pain subsides with growth cessation [5]. The spinal deformity, and subsequently, the self-perceived body image (SPBI) is the most common complaint of patients with Scheuermann’s disease and is typically the primary reason of younger patients that seek medical attention [6]. This parameter is underestimated by several researchers; however, as mentioned before, it is crucial for patients, most of who are at the puberty or post-pubertal age. Many studies have examined the psychological impact associated with scoliosis and kyphosis. These studies have shown that scoliosis patients have a negative body image perception and are therefore more likely to report being less healthy, more worried that their body was developing abnormally, and had greater concerns about the quality of peer relationships [7,8]. Based on our experience, the situation might be similar in Scheuermann’s kyphosis patients.
Very few trials have mentioned physical therapy exercise programs as an effective treatment for Scheuermann’s kyphosis. Although limited evidence is available to show that only physical therapy can change the natural history of Scheuermann’s disease, it is often used as the first choice of treatment. Soo et al. [9] have suggested other important considerations, such as patient age, spinal deformity, and back pain severity, while selecting the appropriate treatment for patients with Scheuermann’s kyphosis. Generally, skeletally immature patients with a kyphotic curve 45° to >50° and radiographic findings of Scheuermann’s disease may be candidates for physical therapy treatment and bracing. Intensive physical therapy exercise programs for postural improvement have been attempted for several years without any conclusive evidence showing that physical therapy alone can lead to kyphotic improvement [3,10]. Moreover, majority of the adults with untreated Scheuermann’s disease respond positively to physical therapy and a back exercise program in cases where the kyphosis is not severe (<60°) [11]. In adolescent patients with Scheuermann’s disease whose kyphosis is >60°, a combined full-time brace program (>20 hours per day) and an exercise program should be considered [12]. Both stretching and strengthening exercises should be prescribed for the trunk as well as tight hamstring and pectoral musculature [13,14].
Our clinical experience and research findings [15] as well as other reports [16,17] suggest that Schroth therapy may be effective in preventing deterioration and decreasing the thoracic angle curve in Scheuermann’s patients. For example, Weiss et al. [16] reported their results of long-term physical therapy, osteopathy, manual therapy, exercise program, and psychological therapy in a group of 351 patients (aged 17–21 years) with painful Scheuermann’s kyphosis. At treatment completion, both the Visual Analog Scale and the Numerical Pain Rating Scales (NPRS) showed significant pain reduction of 16%–32% in all cases.
A three-dimensional exercise therapy program (Schroth therapy) was developed in Germany in the 1920s by Katharina Schroth [18]. This program is based on sensorimotor and kinesthetic principles and incorporates corrective therapeutic exercises, special breathing techniques, and re-education of the neuromuscular system. The treatment program that was customized for each patient included correction of the kyphotic posture with the help of proprioceptive and exteroceptive stimulation and mirror control in the sagittal plane while involving a specific breathing pattern into the rhythm of the practice. These exercises include a combination of forces that produce external forces on the vertebral column. The forces are produced by correction of the three blocks in the sagittal plane together with elongation force on the vertebral column. The main principles of physical exercises are passive and active reduction of the kyphotic hump as well as stretching of the hamstring and pectoralis muscles. The detailed explanations given to patients develop their self-confidence and encourage them to exercise. Motivation and cooperation are essential components of the Schroth method. The initial external force involved in every Schroth exercise is elongation. Using sensorimotor feedback mechanisms, the patients learn individual correction routine. With time, the patients use corrective active trunk muscle forces and learn to raise themselves as far as possible from the slumped position. Thereafter, they are required to maintain the corrected posture while performing daily living activities, automatically resulting in a more erect trunk.
Therefore, we aimed to evaluate the efficacy of the Schroth therapy and compare it to the efficacy of classic anti-gravitation exercises in preventing the deterioration of the thoracic curve angle to reduce the pain level and improve the SPBI of the back in Scheuermann’s disease patients. Consequently, we hypothesized that Schroth therapy treatment is more effective than classic anti-gravitation exercises in terms of improving the abovementioned parameters in these patients.
This study was performed at the Maccabi Hashalom Posture Clinic of the Maccabi Health Care Services in Tel Aviv and the Maccabi Bat-Yam Posture Clinic of the Maccabi Health Care Services in Bat-Yam.
The interventions (studied and control) used in this study are commonly accepted and routinely applied in the management of patients with Scheuermann’s kyphosis. Each patient could discontinue study participation or move from his/her study group and join the other group whenever he/she wanted. No invasive treatments or examinations were performed during the study.
The research proposal was approved by the ethical (Helsinki) committee of Maccabi Healthcare Services (N:2/2015) and the Institutional Review Board of Ben-Gurion University. As custodians, the parents of the patients signed an informed consent form according to the medical ethics laws.
Total 50 young adults (males and females) with Scheuermann’s disease were randomly divided into two groups. Twenty-five participants were assigned to the experimental group (Schroth therapy treatment), and 25 participants were assigned to the control group (classic anti-gravitation exercises). Board-certified orthopedic surgeons established Scheuermann’s disease (International Classification of Diseases 9th Revision, Clinical Modification [ICD-9-CM] diagnosis code 732.0/ICD-10–M42.0) and referred the patients to conservative treatments in the posture clinic. These participants were diagnosed again and treated from 2013–2016 in the Maccabi Hashalom Posture Clinic in Tel Aviv and the Maccabi Bat-Yam Posture Clinic in Bat-Yam of Maccabi Healthcare Services, Israel. Therefore, this sample can be considered as representative of the general population of Scheuermann’s disease patients. Radiography was performed by specially trained technicians using a standard procedure in the department of radiology of the Maccabi Healthcare Services Centers. A relatively new technology of digital radiography was used. All the radiographs were stored in a picture archiving and communication system. This system allows very clear visualization of the mid-thoracic spine in the lateral view and very accurate digital measurements of the Cobb angle. The lateral view radiographs of the whole spinal column were taken in the standing position with straight arms at 90° shoulder flexion. Participants were instructed to stand in a natural position and put equal weight on both the feet. Lateral radiographs were taken before and after the treatment period for each patient.
The inclusion criteria were as follows: (1) age 10–17 years; (2) adolescent Scheuermann–ICD-9-CM diagnosis code 732.0/ICD-10–M42.0; and (3) motivation to perform exercises every day. The exclusion criteria were as follows: (1) participants who were or are being treated with a brace; (2) participants who underwent an orthopedic operation; (3) postural hyperkyphosis; (4) congenital hyperkyphosis; (5) neuromuscular hyperkyphosis; (6) traumatic hyperkyphosis; (7) tumors; and (8) chronic users of pain medication.
The main outcome measure was the Cobb angle of the thoracic kyphosis. The sample size was estimated using on-line Power/Sample Size Calculator (http://www.statisticalsolutions.net/pss_calc.php).
In a previous study by Otman et al. [17], the Cobb angle within each subject group was normally distributed with a standard deviation 5. If the real difference in the experimental and control means was 5, we needed to study 17 experimental subjects and 17 control subjects to reject the null hypothesis that the population means of the experimental and control groups were equal, with a probability (power) of 0.8. Type I error probability associated with this test of this null hypothesis was 0.05. We estimated a dropout rate of 25%; therefore, we recruited 25 subjects in each group.
After applying the inclusion and exclusion criteria and obtaining informed consent, the participants were randomly assigned to either the active or the control group via simple randomization using 50 opaque sealed envelopes prepared and mixed thoroughly before study onset (Fig. 1). For each patient, the consequent sealed envelope was opened that allocated him/her to the control or experimental group.
The following data were collected using the lateral radiographs of the whole spinal column in the standing position.
The thoracic kyphosis angle (T3–T12) was measured using the modified Cobb method. The thoracic Cobb angle was measured from the T3 superior endplate to the T12 inferior endplate (the upper line was drawn at the superior endplate of T3 and the lower line was drawn at the inferior endplate of T12). This method offer good validity and reliability of measurements [19]. The thoracic kyphosis angle was the main outcome measure.
L5-KAL was measured as the distance between the vertical line from the L5 anterior vertebral body to the anterior border of the thoracic kyphosis apex vertebral body. This method was suggested by our group, based on clinical experience, and is now being examined for its validity and reliability.
The following data were collected from the medical files: age, sex, height (measured in a natural standing position using a SECA altimeter [SECA, Hamburg, Germany]), weight, body mass index, family history (positive/negative), child developmental disorders (positive/negative), and Risser sign (0–5; obtained from the pelvic radiographs).
Health-related quality of life: The Scoliosis Research Society-22 Questionnaire (SRS-22) is valid and reliable with internal consistency and reproducibility comparable to that of the 36-item Short-Form Health Survey. It is a well-recognized self-assessment instrument used for the clinical evaluation of patients with adolescent idiopathic scoliosis and other spinal deformities [20]. The questionnaire consists of five domains (function/activity, pain, self-image/appearance, mental health, and satisfaction with management). The health-related quality of life was an additional main outcome measure.
SPBI: The SPBI was evaluated using a numeric scale, ranging from 0 to 10 (from satisfied to very dissatisfied with the appearance). A similar method of SPBI has been validated in others areas of medicine [21].
Pain (NPRS): We measured the degree of pain experienced during the previous week, as measured using the NPRS, with 0 indicating ‘no pain at all’ and 10 indicating ‘the worst possible pain’ [16,22]. Studies have shown that the NPRS scale is a valid and reliable tool for assessing pain in Scheuermann’s patients [9,22].
Shoulder range of motion: The active flexion of the shoulder joint was measured in the supine and standing positions using a digital inclinometer that was a valid and reliable instrument for quantifying shoulder mobility, especially when the clinicians used similar instruments. Excellent interrater reliability was present with intraclass correlation coefficients (≥0.95) [23,24].
Kyphotic deformity: The thoracic kyphosis angle was calculated by the summation of the angle recorded using the digital inclinometer placed over the T1 and T2 spinous processes and the angle recorded using the inclinometer placed over the T12 and L1 spinous processes. The patient was instructed to stand in a normal posture in his natural position during the test. The assessments of anteroposterior curvatures of the spine by one investigator provide good repeatability and reliability of measurements [25]. Other researchers indicated excellent intra-rater reliability in the measurement of thoracic kyphosis using an inclinometer [26,27].
In this study, participants from both the groups received a course of individual treatment sessions for 610 weeks, with one appointment per week. One group was treated with five classic Schroth therapy exercises (Fig. 2), and the second was treated with five classic anti-gravitation exercises (Fig. 3). The Schroth therapy (experimental group) program incorporates corrective therapeutic exercises, special breathing techniques, and re-education of the neuromuscular system. The treatment program involves correction of the kyphotic posture with the help of proprioceptive and exteroceptive stimulation in the sagittal plane. The initial external force involved in every Schroth exercise is elongation. With time, the participants use corrective active trunk muscle forces and learn to raise themselves as far as possible from the slump position, together with the correction the three blocks in the sagittal plane. Thereafter, they need to maintain the corrected posture while performing daily living activities. The exercises include a breathing technique, focusing on improving the rib motion and aiming to increase the patient’s vital capacity. Each exercise was customized for each patient from the intervention group for his specific posture.
The anti-gravitation exercises (control group) involved five classic conventional exercises that refer the whole back and are used routinely in posture clinics for hyperkyphosis treatment. The body is in the prone position (the face is parallel to the floor), and the exercises are performed against the gravitational force.
During each visit, the exercise performance of both the groups was checked by the Schroth therapist who verified the high-quality performance of each exercise by the patient. Following this confirmation, the participants were asked to perform the exercises once a day, 10 repetitions of three sets, with a rest period of 30 seconds between each consequent set. They were required to perform the exercises daily throughout the 1-year study period and to record their performance in a research log. All the patients received extensive verbal explanations about the pathology and the importance of the exercises from the physical therapist. Each participant got an illustrated list of the exercises he/she needs to perform. Each participant was assessed clinically and radiologically before the randomization (first evaluation), at 6 months after beginning the daily exercises program (second evaluation), and at 12 months after the first evaluation (third evaluation) (Fig. 1).
Throughout the study, the examiner was blinded to participant allocation and the participants were unaware regarding their treatment group (double-blinded). (The participants were aware of the type of treatment they received; however, they were unaware of their study group, control or intervention). All the patient evaluations were performed by the assessor (experienced physical therapists who had been performing treatment of spinal deformities for >17 years) who was blinded to patient allocation. The physical therapist who performed the interventions (Schroth therapy or antigravity exercises) was not blinded to the type of treatment. There were no data exchange between the assessor and the physical therapist who performed the interventions.
Statistical analysis was performed using the IBM SPSS software ver. 21.0 for Windows (IBM Corp., Armonk, NY, USA). To compare the demographic and baseline clinical characteristics of the groups, we conducted the following analyses. Continuous variables were compared using independent samples T-test (with Levene’s test for equality of variances). Dichotomous variables were compared using Pearson’s chi-square test. Ordinal variables were compared using Mann-Whitney’s test.
The outcome measures were compared using the mixed analysis of variance (ANOVA) to test for the main effect of time and for an interaction effect between group and time. We found significant differences in the sex, height, and age of the two groups; therefore, we introduced these variables as covariates in the mixed models to adjust for their effect on the outcome measures.
All statistics were conducted using an intention to treat analysis. The effect size was calculated using partial etasquared.
The study sample included 25 participants in the intervention group (mean age, 14.52±1.79 years) and 25 participants in the control group (mean age, 13.39±1.66 years) (Table 1). Finally, 50 participants met the inclusion criteria and were enrolled. Only 44 subjects completed the study; three dropped out from the control group because they were unable to visit the clinic, one was excluded from the intervention group because of the start of brace treatment, and two additional participants from the intervention group were excluded because of extremely high values of thoracic kyphosis relative to the sample distribution in their last measurement (outliers).
When we compared the demographic and baseline characteristics of the groups (Table 1), we found no significant differences in most parameters, except for age (14.52±1.79 years versus 13.39±1.66 years), height (1.63±0.11 m versus 1.56±0.09 m), kyphotic deformity measured using an inclinometer (59.45°±7.65° versus 54.04°±6.71°), and sex (63.6% versus 20% males) (p<0.05).
In the mixed ANOVA, the main effect of time was significant in thoracic kyphosis (F [1]=5.72, p=0.02) and L5-KAL (F [1]=5.76, p=0.02) (Table 2). The main effect of time on kyphotic deformity measured using an inclinometer did not reach a significant level; however, it showed such a tendency (F [1]=2.80, p=0.07). In the group-by-time interaction, a significant difference was found in thoracic kyphosis (F [1]=4.91, p=0.03) and in the kyphotic deformity measured using an inclinometer (F [1]=4.05, p=0.02), indicating that the Schroth therapy group showed significantly greater improvement than the classic anti-gravitation exercises group in this study.
Within-group tests for measuring the change in the outcome measures indicated significant changes over time in the shoulder flexion (supine and standing), kyphotic deformity measured using an inclinometer, SRS-22, and thoracic kyphosis (p<0.01). Body image improved significantly only in the intervention group (p<0.01), while no significant change was observed in the control group (p=0.70). Pain in the last week improved significantly only in the control group (p=0.05), while no significant change was observed in the intervention group (p=0.30).
The mean improvement in the thoracic kyphosis in the control group was 3.57º±7.59º, while that in the intervention group was 8.78º±8.38º. Further, the mean improvement in the kyphotic deformity measured using an inclinometer in the control group was 4.09º±6.71º, while that in the intervention group was 10.54º±7.65º.
During the previous decade, Schroth therapy has become one of the most common conservative treatments for spinal deformities in Western countries, with no strong evidence for its effectiveness. We performed a randomized controlled single-blinded clinical trial on 50 Scheuermann’s disease patients with thoracic kyphosis Cobb angle of 47°–81º who were treated in the special clinic of the second largest healthcare provider in the central district of Israel. Our study population only comprised patients who were referred for special physical therapy; therefore, we can assume that our study population represented the population of Scheuermann’s disease patients in the central district of Israel. The subjects were examined for any changes in the thoracic Cobb angle, pain during the previous week, body image, L5-KAL, shoulder flexion in the supine and standing positions, kyphotic deformity measured using an inclinometer, and SRS-22. Our present findings provide initial evidence regarding the effectiveness of physical therapy in general and of Schroth therapy in particular. The within-group calculations in both groups showed significant improvements in the shoulder flexion (supine and standing), kyphotic deformity measured using an inclinometer, SRS-22, and thoracic kyphosis Cobb angle. The results of mixed ANOVA showed a significant effect of time on thoracic kyphosis and L5-KAL.
A significant effect of group-by-time interactions found in our study for thoracic kyphosis, measured using both the Cobb angle and an inclinometer, provided an initial evidence that Schroth exercises are more effective than anti-gravitation exercises in improving thoracic kyphosis in adolescent Scheuermann’s disease patients. We believe that the higher efficacy of the Schroth method as compared to that of the conventional antigravity exercises is mainly attributable to the following three factors: First, the elongation force that is very unique to Schroth therapy is crucial for the postural correction. Second, patients treated using the Schroth method were instructed to maintain the corrected posture while performing their daily living activities; this amplified the treatment time. Finally, although all the patients in the Schroth therapy group performed the same five exercises, each exercise was tailored individually for each patient as per his/her posture.
Our results are supported by two previous case reports and one randomized controlled trial (RCT). The first case report describes a 14-year-old girl with Scheuermann’s disease whose thoracic kyphosis Cobb angle improved from 55º to 27º after a 7-week course of Schroth therapy sessions with daily home exercises tailored specifically for her posture [15]. Improvement was also documented for SPBI, lumbar lordosis, and C7 line. Another case report was that of a 76-year-old woman who performed Schroth exercise sessions thrice a week for 6 months [28]. In addition, she was recommended a home exercise program. She also wore a SpinoMed brace for 2 hours every day. After a 6-month treatment period, her kyphosis Cobb angle was reduced from 85° to 70°, and a recent radiograph taken 1 year thereafter showed another improvement in the sagittal plane, with thoracic kyphosis measuring 64°. The improvement was also been documented for the lumbar lordosis Cobb angle and for the pain score.
This study has certain limitations. First, the study sample was relatively small and influenced the demographic and baseline clinical characteristics. Second, we could not predict the effect of the natural evaluation of the deformity because of the inability to create a control group that was not given treatment. Third, most subjects had mild to moderate deformities; there were few severe cases, thus the findings are only applicable to a limited population. Fourth, the kyphotic deformity measured using the inclinometer was significantly larger in the intervention group than in the control group; however, we believe that this did not influence our results. Moreover, the kyphotic deformity assessed using an inclinometer was not the main outcome measure.
When we estimated the sample size using the data from the study by Otman et al. [17], we found that 17 participants in each group would be sufficient to reject the null hypothesis. Thus, we decided to recruit 25 participants in each group. However, the standard deviations of the main outcome measure (thoracic kyphosis as per the Cobb angle) in our study were much higher than the ones in the study of Otman et al. [17]. When we calculated the statistical power using the obtained difference and the standard deviations of the thoracic kyphosis as per the Cobb angle, we found that the statistical power of our study was low. We believe that in a larger sample, more outcome measures will show a significant difference.
This RCT indicates that a physical therapy exercise program in general, and the Schroth therapy in particular is an effective treatment for preventing and improving the thoracic Cobb angle and reducing the symptomatic representation in Scheuermann’s patients. Schroth therapy is a preferable method as compared to classic anti-gravitation exercises. These results provide the clinicians with more accurate tools for treating patients with Scheuermann’s disease. Other prospective controlled clinical trials with longer follow-up duration and a larger group of Scheuermann’s patients are needed to investigate the influence of conservative treatments on other important parameters, such as the pulmonary function (vital capacity) and the state of mind.
Future studies are warranted to investigate the crucial parameter of SPBI and create a relative practical assessment tool.
Fig. 2.
Experimental group: five exercises of Schroth therapy. (A) Pendulum; (B) corrections in supine-elbows against the floor; (C) semihanging; (D) corrections in sitting: forearms against the knees; and (E) corrections in standing–against elastic bands.
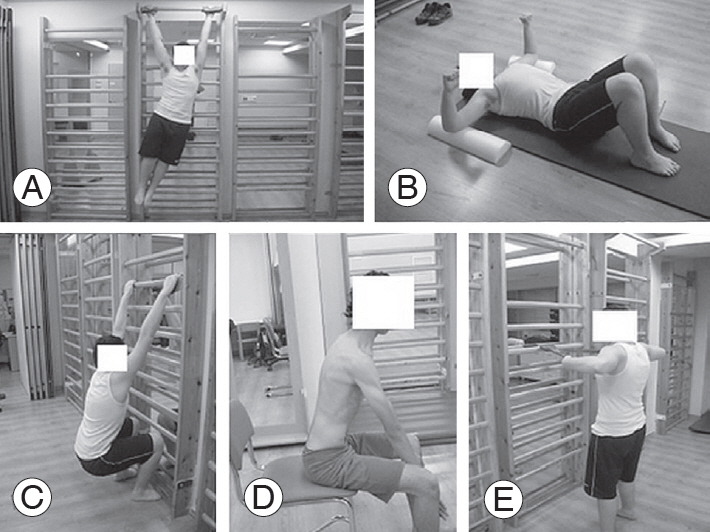
Fig. 3.
Control group: five classic anti-gravitation exercises. (A) Superman; (B) shoulder scapular retraction; (C, D) back extension; and (E) back strengthening–bird dog exercise.
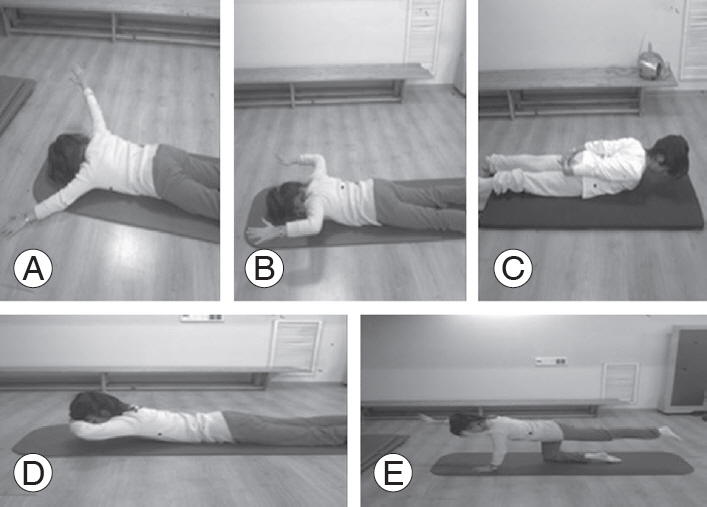
Table 1.
Demographic and baseline clinical characteristics of the studied sample
| Characteristic | Intervention group (N=25) | Control group (N=25) | Comparisona) |
|---|---|---|---|
| Continuous variable | |||
| Age (yr) | 14.52±1.79 | 13.39±1.66 | t =-2.24, p =0.03 |
| Height (m) | 1.63±0.11 | 1.56±0.09 | t =-2.22, p =0.03 |
| Weight (kg) | 51.89±11.95 | 49.65 ±12.24 | t =-0.63, p =0.53 |
| Body mass index (kg/m2) | 19.38±3.37 | 20.12±3.82 | t =0.70, p =0.48 |
| Thoracic kyphosis (°) | 60.18±8.38 | 56.16 ±7.59 | t =-1.72, p =0.09 |
| L5-kyphosis apex line (cm) | 11.78±2.91 | 11.64±2.48 | t =-0.15, p =0.88 |
| Flexion of shoulder supine (°) | 168.05±9.46 | 165.96±9.22 | t =-0.76, p =0.45 |
| Flexion of shoulder standing (°) | 156.91±12.31 | 157.12±13.88 | t =0.05, p =0.96 |
| Kyphotic deformity Inclinometer (°) | 59.45±7.65 | 54.04±6.71 | t =-2.58, p =0.01 |
| Scoliosis Research Society-22 Questionnaire | 42.27±7.92 | 42.64±6.33 | t =0.18, p =0.86 |
| Categorical variable | |||
| Sex (males) | 63.6 | 20 | χ2=9.25, p<0.01 |
| Genetics (positive) | 36.4 | 44 | χ2=0.28, p =0.59 |
| Child developmental disorders (negative) | 86.4 | 88 | χ2=0.03, p =0.87 |
| Ordinal variable | |||
| Risser sign | 2 (1–4) | 2 (0.25–4) | Z =-0.03, p =0.97 |
| Pain in last week (Numerical Pain Rating Scale) | 2 (0–4.25) | 2 (0–5) | Z =-0.46, p =0.64 |
| Self-perceived body image (Numeric Rating Scale) | 5 (2.25–7) | 3 (0–6) | Z =-1.31, p =0.19 |
Table 2.
Summary of findings for group-by-time interaction
| Variable | Group | Baseline | End of treatment | Group-by-time interaction | Main effect of time |
|---|---|---|---|---|---|
| Paina) (0–10) (Numerical Pain Rating Scale) | Intervention group | 2.24±2.40 | 1.2±1.94 | Z=-0.42, p=0.68 | |
| Control group | 2.91±3.02 | 1.45±2.04 | |||
| Self-perceived body imagea) (0–10) (Numerical Rating Scale) | Intervention group | 4.80±3.27 | 2.72±2.09 | Z=-1.51, p=0.13 | |
| Control group | 2.59±3.35 | 1.64±1.92 | |||
| Thoracic kyphosisb) (°) | Intervention group | 60.18±8.38 | 51.40±7.64 | F (1)=4.91, p=0.03 (partial η²=0.11) | F (1)=5.72, p=0.02 |
| Control group | 54.71±5.57 | 51.14±5.80 | |||
| L5-kyphosis apex lineb) (cm) | Intervention group | 11.78±2.91 | 10.28±2.84 | F (1)=1.32, p=0.26 (partial η²=0.04) | F (1)=5.76, p=0.02 |
| Control group | 11.32±2.35 | 10.68±3.16 | |||
| Flexion shoulder supine (°) | Intervention group | 168.05±9.46 | 171.82±7.15 | F (1)=2.15, p=0.14 (partial η²=0.02) | F (1)=1.11, p=0.31 |
| Control group | 167.55±8.54 | 170.10±7.21 | |||
| Flexion shoulder standing (°) | Intervention group | 156.91±12.31 | 167.27±9.63 | F (1)=0.92, p=0.39 (partial η²=0.02) | F (1)=0.05, p=0.94 |
| Control group | 159.23±13.43 | 166.27±10.30 | |||
| Kyphotic deformity by inclinometer (°) | Intervention group | 59.45±7.66 | 48.91±4.95 | F (1)=4.05, p=0.02 (partial η²=0.09) | F (1)=2.80, p=0.07 |
| Control group | 53.14±6.18 | 49.05±7.19 | |||
| Scoliosis Research Society-22 items Questionnaire | Intervention group | 42.27±7.92 | 33.68±6.91 | F (1)=1.87, p=0.17 (partial η²=0.04) | F (1)=0.18, p=0.76 |
| Control group | 42.64±6.33 | 32.24±13.98 |
References
1. Holt RT, Dopf CA, Isaza JE,Adult kyphosis. Frymoyer JW, editors. The adult spine: principles and practice. Philadelphia (PA): Lippincott Williams&Wilkins; 1997. p.1537–78.
2. Graat HC, van Rhijn LW, Schrander-Stumpel CT, van Ooij A. Classical Scheuermann disease in male monozygotic twins: further support for the genetic etiology hypothesis. Spine (Phila Pa 1976) 2002 27:E485–7.


4. Murray PM, Weinstein SL, Spratt KF. The natural history and long-term follow-up of Scheuermann kyphosis. J Bone Joint Surg Am 1993 75:236–48.


6. Bradford DS, Moe JH, Montalvo FJ, Winter RB. Scheuermann’s kyphosis and roundback deformity: results of Milwaukee brace treatment. J Bone Joint Surg Am 1974 56:740–58.


7. Sapountzi-Krepia DS, Valavanis J, Panteleakis GP, Zangana DT, Vlachojiannis PC, Sapkas GS. Perceptions of body image, happiness and satisfaction in adolescents wearing a Boston brace for scoliosis treatment. J Adv Nurs 2001 35:683–90.


8. Payne WK 3rd, Ogilvie JW, Resnick MD, Kane RL, Transfeldt EE, Blum RW. Does scoliosis have a psychological impact and does gender make a difference? Spine 1997 22:1380–4.


10. Bradford DS, Ahmed KB, Moe JH, Winter RB, Lonstein JE. The surgical management of patients with Scheuermann’s disease: a review of twenty-four cases managed by combined anterior and posterior spine fusion. J Bone Joint Surg Am 1980 62:705–12.


12. Lings S, Mikkelsen L. Scheuermann’s disease with low localization: a problem of under-diagnosis. Scand J Rehabil Med 1982 14:77–9.

13. Sachs B, Bradford D, Winter R, Lonstein J, Moe J, Willson S. Scheuermann kyphosis: follow-up of Milwaukee-brace treatment. J Bone Joint Surg Am 1987 69:50–7.


14. Montgomery SP, Erwin WE. Scheuermann’s kyphosis: long-term results of Milwaukee braces treatment. Spine 1981 6:5–8.


15. Bezalel T, Kalichman L. Improvement of clinical and radiographical presentation of Scheuermann disease after Schroth therapy treatment. J Bodyw Mov Ther 2015 19:232–7.


16. Weiss HR, Dieckmann J, Gerner HJ. Effect of intensive rehabilitation on pain in patients with Scheuermann’s disease. Stud Health Technol Inform 2002 88:254–7.

17. Otman S, Kose N, Yakut Y. The efficacy of Schroth s 3-dimensional exercise therapy in the treatment of adolescent idiopathic scoliosis in Turkey. Saudi Med J 2005 26:1429–35.

18. Lehnert-Schroth C. Introduction to the three-dimensional scoliosis treatment according to Schroth. Physiotherapy 1992 78:810–5.

19. Greendale GA, Nili NS, Huang MH, Seeger L, Karlamangla AS. The reliability and validity of three non-radiological measures of thoracic kyphosis and their relations to the standing radiological Cobb angle. Osteoporos Int 2011 22:1897–905.


20. Asher M, Min Lai S, Burton D, Manna B. The reliability and concurrent validity of the scoliosis research society-22 patient questionnaire for idiopathic scoliosis. Spine 2003 28:63–9.


21. Larsson P, John MT, Nilner K, List T. Reliability and validity of the Orofacial Esthetic Scale in prosthodontic patients. Int J Prosthodont 2010 23:257–62.

22. Ristolainen L, Kettunen JA, Heliovaara M, Kujala UM, Heinonen A, Schlenzka D. Untreated Scheuermann’s disease: a 37-year follow-up study. Eur Spine J 2012 21:819–24.


23. Kolber MJ, Vega F, Widmayer K, Cheng MS. The reliability and minimal detectable change of shoulder mobility measurements using a digital inclinometer. Physiother Theory Pract 2011 27:176–84.


24. Kolber MJ, Hanney WJ. The reliability and concurrent validity of shoulder mobility measurements using a digital inclinometer and goniometer: a technical report. Int J Sports Phys Ther 2012 7:306–13.


25. Czaprowski D, Pawłowska P, Gebicka A, Sitarski D, Kotwicki T. Intra- and interobserver repeatability of the assessment of anteroposterior curvatures of the spine using Saunders digital inclinometer. Ortop Traumatol Rehabil 2012 14:145–53.


26. Lewis JS, Valentine RE. Clinical measurement of the thoracic kyphosis: a study of the intra-rater reliability in subjects with and without shoulder pain. BMC Musculoskelet Disord 2010 11:39.




- TOOLS







